What’s so special about anaesthesia meds?
Anaesthesia medications are some of the most effective and deadly medications available for human consumption. Fortunately when used by an anaesthetist, they are remarkable safe and effective. Through the 5 years of formal anaesthesia training you end up using a unique group of medications on a daily basis and develop immense familiarity with their use and how to manage the common side effects and rare deadly complications. For these reasons, very few doctors use these medications.
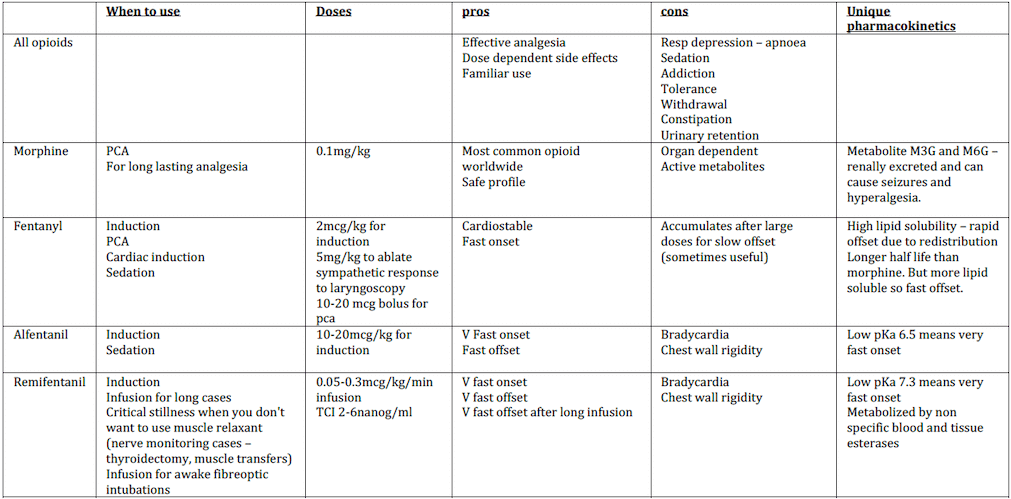
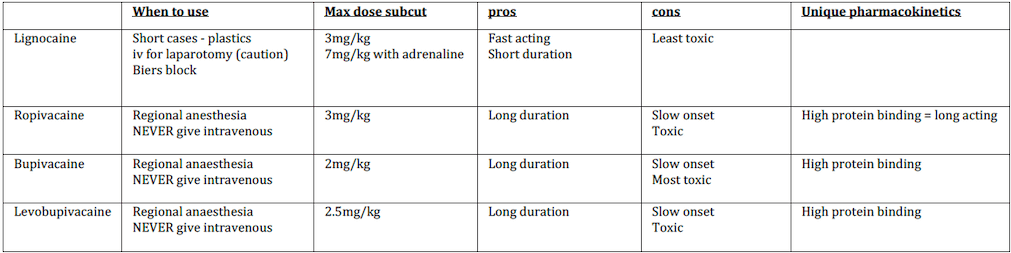
We also have to pass 2 very difficult exams that test us on incredibly detailed aspects of these meds like these:
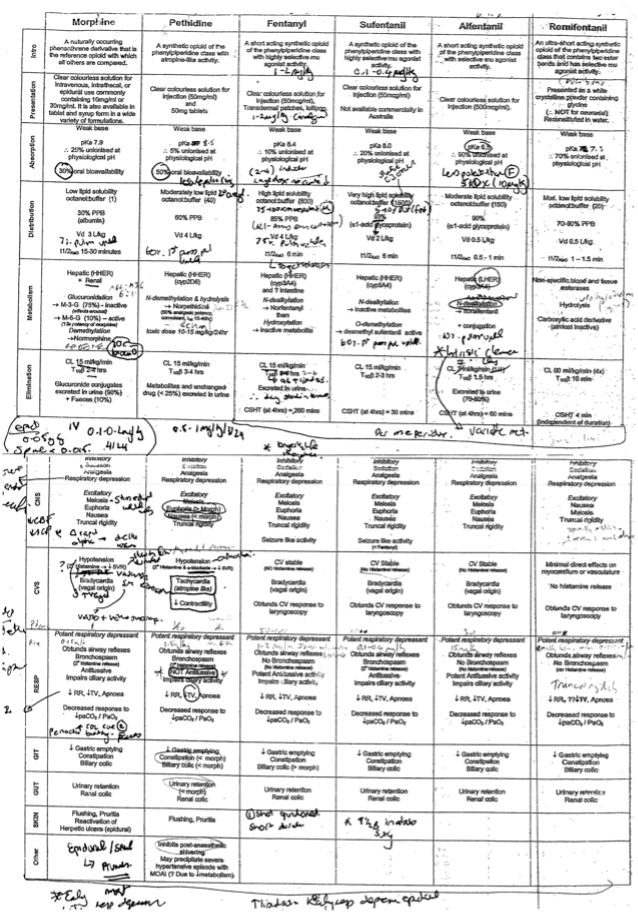
Scary right? But don’t worry, now I realise that to use these medications safely you don’t need to know the hundreds of little details like pKa, protein binding or clearance rate. You just need to know a few points of different, a few hacks that anaesthetists use when making decisions.
In this article I want to give anaesthesia trainees a hack/focused guide to using these incredible medications. Essentially this means covering all the things that actually matter for the day-to-day use without all the minutiae!
- When to use them
- Doses
- Favorable characteristics
- Reasons to be cautious
- And the really serious complications
- Useful tips
So what are these classes of medications?
- Intravenous induction agents
- Volatile hypnotics agents
- Muscle relaxants
- Opioids
- Local anaesthetics
IV induction agents
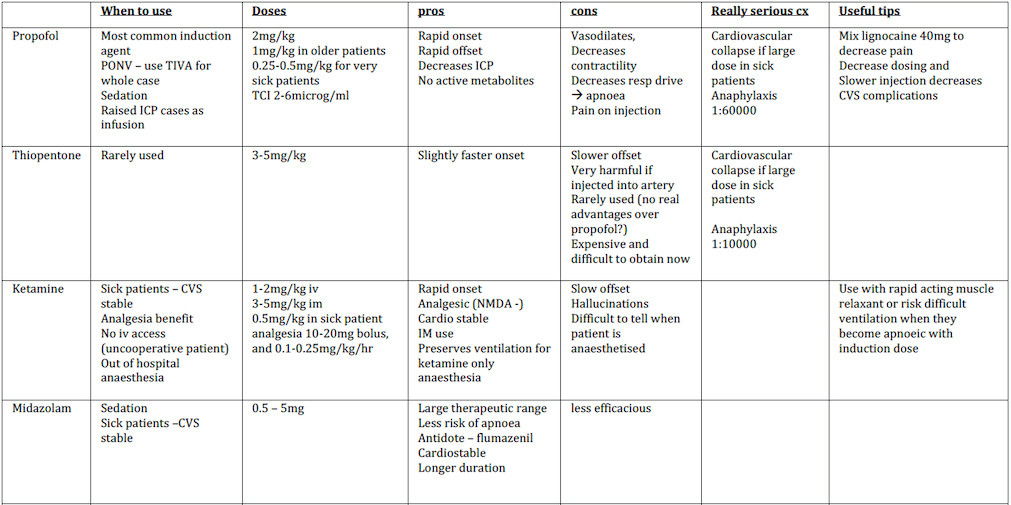
What iv induction agent would you use?
- 50yo 70kg male with no medical issues need a laparoscopic cholecystectomy
- 40yo 80kg female patient presents for laparoscopic ovarian cystectomy. She has previously had severe PONV lasting for 2 days.
- 60yo 80kg patient for cardiac bypass surgery, has had recent major AMI and blocked LAD and Left circumflex arteries now with decreased LV ejection fraction of 30%.
- 21yo 70kg male for emergency laparotomy after motor vehicle accident. Bp 70/60, HR 130 and GCS 10 with suspected 3L blood loss.
Volatile agents
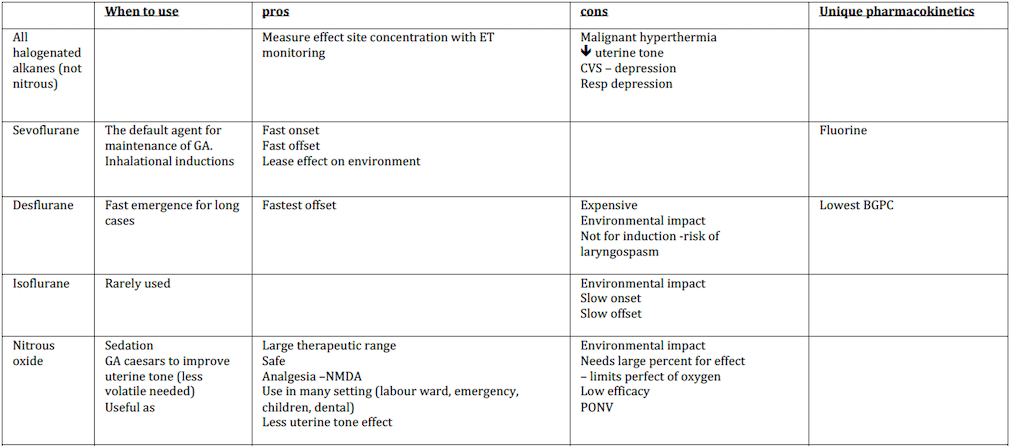
What inhalational agent would you use?
- 50yo male with no medical issues presents for a laparoscopic cholecystectomy
- 30yo female patient requests analgesia for labour
- The previous patient needs an emergency GA Caesar.
- A patient needs a long craniotomy for brain tumour
- 70yo patient with severe cardiac disease and end stage renal failure has an axillary nerve block for radiocephalic AV fistula. The patient starts to feel some pain in the middle of the case but you have used the maximum amount of local anaesthetic allowed. You don’t want to give a full GA because of the patients comorbidities
- 20yo patient for an emergency appendicectomy tells you he has a family history of malignant hyperthermia.
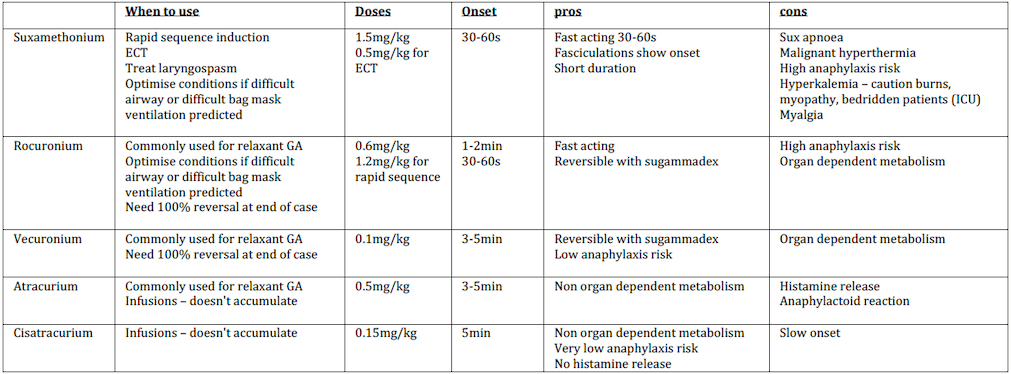
Muscle relaxants
What muscle relaxant would you use?
- 50yo male with no medical issues presents for a laparoscopic cholecystectomy
- 60yo female with small bowel obstruction for emergency laparotomy
- 30yo female for long craniotomy. Surgeons require a very still operative field
- 50yo male needs GA for bowel resection for cancer. Had anaphylaxis during a previous anaesthetic 20 years ago. Never tested.
- 40yo male with large beard and obstructive sleep apnoea (OSA) for a tonsillectomy.
- 20yo female asthmatic for diagnostic laparoscopy.
- 1yo child is undergoing inhalational induction for lip laceration repair. She has laryngospasm and her sats decrease to 50% as you are unable to oxygenate, ventilate or obtain iv access.
- 60yo female with small bowel obstruction for emergency laparotomy. Just arrived on ward after being in ICU bedridden for 3 months with pneumonia and respiratory failure.
- 60yo female for a laparoscopic hysterectomy. Has chronic renal impairment eGFR 20.
Useful tips
When to reverse?
Usually a patient is ready to reverse paralysis with neostigmine 0.05mg/kg (2.5mg) and glycopyrrolate 5mcg/kg (400mcg) when they have 2-3 twitches present on train of four monitoring. This causes and increase in ACh at the neuromuscular junction displacing the muscle relaxant and allowing recovery of muscle function. Sugammadex directly bind to the rocuronium or vecuronium so doesn’t need recovery of twitches before administration. However deeper levels of muscle paralysis will need larger doses of sugammadex.
Opioids
What opioid would you use?
- 50yo male with no medical issues presents for a laparoscopic cholecystectomy
- 60yo female with small bowel obstruction for emergency laparotomy
- 50yo female for thyroidectomy
- 30yo female for long craniotomy. Surgeons require a very still operative field
- 50yo male with known difficult airway, impossible bag mask ventilation and grade 4
intubation previously. LMA ventilation no known. What would you do for the awake fibreoptic intubation? - 80yo for cataract operation. Wants sedation for the case.
- 90yo patient for BCC excision from lip. Multiple comorbidities so want to avoid GA.
- 50yo male for cardiac bypass surgery
Useful tips
Reversal agent
Opioid use creates a high risk of sedation and respiratory depression with apnoea as a potential consequence. The availability of naloxone dramatically enhances safety. Doses of 0.5-1mcg/kg can be given for unwanted respiratory depression and deep sedation. For respiratory arrest given a full 400mcg may be needed and can be given iv/sc/im.
NB that it has a short duration of action, longer than many opioids and it may have to be re-administered.
Local Anaesthetics
What local anaesthetic would you use?
- 20yo female for finger laceration
- 50yo male for supraclavicular brachial plexus nerve block for shoulder reconstruction
- 60yo female for femoral nerve block for total knee replacement
- 80yo male with rib fractures for paravertebral catheter
- 30yo female for labour epidural
- 70yo female with end stage renal failure for radiocephalic AV fistula formation.
- 60yo post laparotomy for TAP blocks
- The surgeons asks for 1% lignocaine with adrenaline but the hospital only stocks 1% lignocaine plain.
Useful tips
Adding adrenaline
1:200 000 adrenaline is 5mcg/ml. This is a common amount in many lignocaine and bupivacaine solutions.
If you want to make a 1:200 000 solution of something you just need to add adrenaline so the final concentration is 5mcg/ml
In the example above, the surgeon asks for 1% lignocaine with adrenaline but the hospital only stocks lignocaine. You can take 20ml of 1% lignocaine, and add 100mcg of adrenaline to make 5mcg/ml adrenaline.
100mcg is either 1 ml of 1:10 000 adrenaline (the big 10ml vial)
OR
0.1ml of the 1:1000 adrenaline (the small 1ml vial)
Always check with someone else when you do unfamiliar or complex dilutions with dangerous substances.
How to calculate max dose by volume
The max dose in ml for 0.75% ropivacaine or 0.5% bupivacaine is 0.4ml/kg.
What does % actually mean?
x% of a solution = 10x mg/ml
so 1% lignocaine = 10mg/ml
0.75% ropivacaine = 7.5mg/ml
If you are in doubt, check the vial and it will give you the percent of solution AND the total mg in the vial.

ANSWERS
What iv induction agent would you use?
1. 50yo 70kg male with no medical issues need a laparoscopic cholecystectomy
I would choose propofol at 150mg and titrated to effect for induction.
2.40yo 80kg female patient presents for laparoscopic ovarian cystectomy. She has previously have severe PONV lasting for 2 days.
I would run propofol TCI at 4-6mcg/ml plasma concentration. I would additionally give 4mg dexamethasone after induction and have ondansetron and droperidol available PRN post op.
3. 60yo 80kg patient for cardiac bypass surgery, has had recent major AMI and blocked LAD and Left circumflex arteries with now decreased LV ejection fraction of 30%.
I would give 3-5mg of midazolam and 300-400mcg of fentanyl titrated slowly during the induction phase. Once the patient was unresponsive I would commence gentle ventilation with Sevoflurane and paralyse the patient.
4. 21yo 70kg male for emergency laparotomy after motor vehicle accident. Bp 70/60, HR 130 and GCS 10 with suspected 3L blood loss
With fluids/blood running through a large IV, I would give 40mg ketamine, 2mg midazolam and 100mg of suxamethonium with metaraminol running and adrenaline ready.
What inhalational agent would you use?
1. 50yo male with no medical issues presents for a laparoscopic cholecystectomy
I would use Sevoflurane for maintenance with an adequate MAC.
2. 30yo female patient requests analgesia for labour
I would offer a number of approaches. Nitrous would be a fast safe primary measure.
3. The previous patient needs an emergency GA Caesar.
I would use Sevoflurane maintenance at a lower concentration supplemented with approx 50% nitrous/oxygen mix to maintain uterine tone. If there is an issue with bleeding due to uterine atony I would switch to propofol TIVA for maintenance of anaethesia
4. A patient needs a long craniotomy for brain tumour
I may use Desflurane at low flows to facilitate rapid awakening.
(That being said I rarely use Desflurane due to it’s severe impact on as an ozone depleting gas and would often prefer Sevoflurane or propofol TIVA).
5. 70yo patient with severe cardiac disease and end stage renal failure has a axillary nerve block for radiocephalic AV fistula. The patient starts to feel some pain in the middle of the case but you have used the maximum amount of local anaesthetic allowed. You don’t want to give a full GA because of the patients comorbidities
After asking the patient to cease operating, I would titrate small doses of an opioid (alfentanil/fentanyl), give 50-70% nitrous, and potentially small doses of midazolam and ketamine depending on how satisfactory my first measures were.
(In reality you may need to proceed to a cautious GA depending on the situation and you may request the surgeon to give further small doses of lignocaine with adrenaline appreciated the risk benefit of doing so)
6. 20yo patient for an emergency appendicectomy tells you he has a family history of malignant hyperthermia.
I would use a ‘non triggering anaesthetic’ following MHANZ http://malignanthyperthermia.org.au guidelines, using propofol TIVA for induction and maintenance of anaesthesia
What muscle relaxant would you use?
1. 50yo male with no medical issues presents for a laparoscopic cholecystectomy
I would use vecuronium (a range of anaesthetists would use any of the non depolarizing muscle relaxants, ie not sux)
2. 60yo female with small bowel obstruction for emergency laparotomy
After ensuring the potassium is normal, I would choose suxamethonium.
(many would use 1.2mg/kg of rocuronium)
3. 30yo female for long craniotomy. Surgeons require a very still operative field
I would induce with atracurium and run an infusion of cisatracurium at 0.5mg/kg/hr and use the neuromuscular monitor.
OR I would induce with rocuronium/vecuronium and run and infusion or use intermittent bolus doses guided by a neuromuscular monitor
OR I would induce with rocuronium/vecuronium/atracurium and use remifentanil to maintain a still patient.
4. 50yo male needs GA for bowel resection for cancer. Had anaphylaxis during a previous anaesthetic 20 years ago. Never tested.
Assuming I cannot delay the surgery for anaphylaxis testing, I would use cisatracurium for its very low anaphylaxs rate.
Other may argue vecuronium also has a low rate of anaphylaxis (but this could be due to its less prevalent use)
5. 40yo male with large beard and obstructive sleep apnoea (OSA) for a tonsillectomy.
I would use rocuronium for its fast onset (so I decrease/eliminate the need to bag mask ventilate- this can be difficult/impossible to do if someone has a beard) and additionally I can directly reverse the patient to ensure his has optimal respiratory function (in light of his OSA)
6. 20yo female asthmatic for diagnostic laparoscopy.
I would use rocuronium or vecuronium. These procedures can be very quick and you may need to reverse with a direct reversal agent (sugammadex).
Prior to having a direct reversal available, intubating conditions were made satisfactory by using a smaller dose of rocuronium and waiting longer for it to work + larger dose of opioid + larger dose of propofol. Using a smaller dose of rocuronium (ED95 of 0.3mg/kg) allowed reversal to be possible sooner in such a fast case.
I would avoid atracurium due to histamine release increasing bronchospasm risk.
7. 1yo child is undergoing inhalational induction for lip laceration repair. She has laryngospasm and her sats decrease to 50% as you are unable to oxygenate, ventilate or obtain iv access.
After sending for immediate help I would give im suxamethonium at 4mg/kg to gain control of the airway.
8. 60yo female with small bowel obstruction for emergency laparotomy. Just arrived on ward after being in ICU bedridden for 3 months with pneumonia and respiratory failure.
I would avoid suxamethonium due to the increase risk of hyperkalemia. I would induce with 1.2mg/kg of rocuronium.
9. 60yo female for a laparoscopic hysterectomy. Has chronic renal impairment eGFR 20.
I would use atracurium as it has non organ dependent metabolism.
What opioid would you use?
1. 50yo male with no medical issues presents for a laparoscopic cholecystectomy
There are many correct options for this case with a large variety in what anaesthetists do. Some would induce with alfentanil and give longer lasting analgesia with morphine or fentanyl. Others would induce and give further analgesia with only fentanyl.
2. 60yo female with small bowel obstruction for emergency laparotomy
I would induce with fentanyl and use fentanyl for further analgesia. She will need multimodal analgesia post op including a fentanyl PCA. (others may induce with alfentanil/fentanyl and continue with morphine and morphine PCA).
3. 50yo female for thyroidectomy
I would use remifentanil throughout the case to avoid the need for muscle paralysis to facilitate recurrent laryngeal nerve monitoring. (this can also be done by using muscle paralysis and ensuring it has been cleared prior to surgeons nerve monitoring)
4. 30yo female for long craniotomy. Surgeons require a very still operative field
I would run remifentanil for the case to facilitate a very still patient throughout the case. (again many ways to do this, including running a muscle relaxant infusion with nerve monitoring or deep anaesthesia – but this might increase ICP)
5. 50yo male with known difficult airway, impossible bag mask ventilation and grade 4
intubation previously. LMA ventilation no known. What would you do for the awake fibreoptic intubation?
I would use a combination of topicalisation with local anaesthetic and opioid to decrease cough reflex and increase tolerance of the procedure. I run remifentanil at 0.05-0.1 mcg/kg/min. (others use alfentanil or fentanyl in bolus doses)
6. 80yo for cataract operation. Wants sedation for the case.
Would use small doses of fentanyl (25-50mcg). You could use small doses of alfentanil but this might increase the risk of apnoea due to its faster onset.
7. 90yo patient for BCC excision from lip. Multiple comorbidities so want to avoid GA.
I would use carefully titrated doses of alfentanil for its fast onset and fast offset. (250mcg)
8. 50yo male for cardiac bypass surgery
I would use up to 5mcg/kg of fentanyl for induction followed by further doses of fentanyl.
What local anaesthetic would you use?
1. 20yo female for finger laceration
I would use lignocaine without adrenaline.
2. 50yo male for supraclavicular brachial plexus nerve block for shoulder reconstruction
I would use 20ml of 0.375% ropivacaine for long lasting sensory block with minimal motor block. Some would use 20ml of 0.75% ropivacaine.
3. 60yo female for femoral nerve block for total knee replacement
I would use 20ml of 0.375% ropivacaine for long lasting sensory block with minimal motor block. Some would use 20ml of 0.75% ropivacaine.
4. 80yo male with rib fractures for paravertebral catheter
I would start with 40ml of 0.375% ropivacaine. And run an infusion of 0.125-0.25% bupivacaine with boluses as per local hospital guidelines.
5. 30yo female for labour epidural
I would commence analgesia with up to 20ml of 0.2% ropivacaine followed by patient controlled epidural analgesia (PCEA) boluses with 0.2% ropivacaine and 2mcg/ml fentanyl as per local hospital guidelines. (usually 5ml bolus q15mins max 60ml in 4 hrs).
6. 70yo female with end stage renal failure for radiocephalic AV fistula formation.
I would use a mixture of 2% lignocaine and 0.75% ropivacaine for a fast onset longer lasting block. (many ways of doing this depending on hospital and surgeon speed).
7. 60yo post laparotomy for TAP blocks
I would use approx. 40ml of 0.375% ropivacaine for a large volume block to spread across the fascial plane. Nerve blocks need less volume as the effect site ie nerve bundle is a more localized area.
8. The surgeons asks for 1% lignocaine with adrenaline but the hospital only stocks 1% lignocaine plain.
I would take 20ml of 1% lignocaine and add 100mcg of adrenaline to make 1% lignocaine with 1:200000 adrenaline. See tips below.
Summary
There is a wide range of options for many of the examples outlined. Consultants choose one medication over another not necessarily because the evidence for its use is better. It may be familiarity, expense, environmental concerns or the pattern of use with consideration of the other agents selected for a case.
There’s often only a few points of difference for each medication that determines its benefit or another so try to use the tables above in your selections.
Every time you select a medication give reason for its use to gain familiarity with the pros and cons of each medication.
Glossary
PONV postoperative nausea and vomiting
TCI target controlled infusion. Enter age and weight, syringe driver then allows you to target and plasma or effect site concentration using pharmacokinetic modeling.
ICP intracranial pressure
TIVA total intravenous anaesthesia
GA general anaesthesia