Click here to download this as a PDF file.
Aim
- To give you a step by step system to choose how to ventilate your patients
- To give you some information about ventilation of the sickest lungs as some principles may apply to healthy lungs as well
Terminology
Tidal volume (Vt) – volume of one breath
Minute ventilation (MV) – total volume of respiration in 1 minute
Respiratory rate (RR) – number of breaths per minute
Positive End Expiratory Pressure (PEEP) – the pressure in the lungs that exists at the end of expiration.
Inspiratory: expiratory Ratio (I:E) – the ratio of time spent in inspiration to expiration. Usually set at 1:2 per 5 second IE cycle. (1.66: 3.33)
Inspiratory pause – interval from the end of inspiratory flow to the start of expiratory flow. Often as a percentage of inspiratory time.
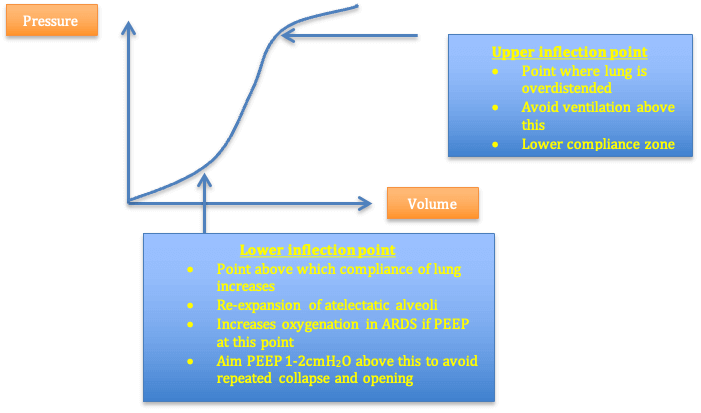
Compliance – a measure of the distensibility of the lung. Shows a sigmoidal curve whereby at low and high lung volumes, the compliance is low. Lung volumes around functional residual capacity (FRC) have high compliance
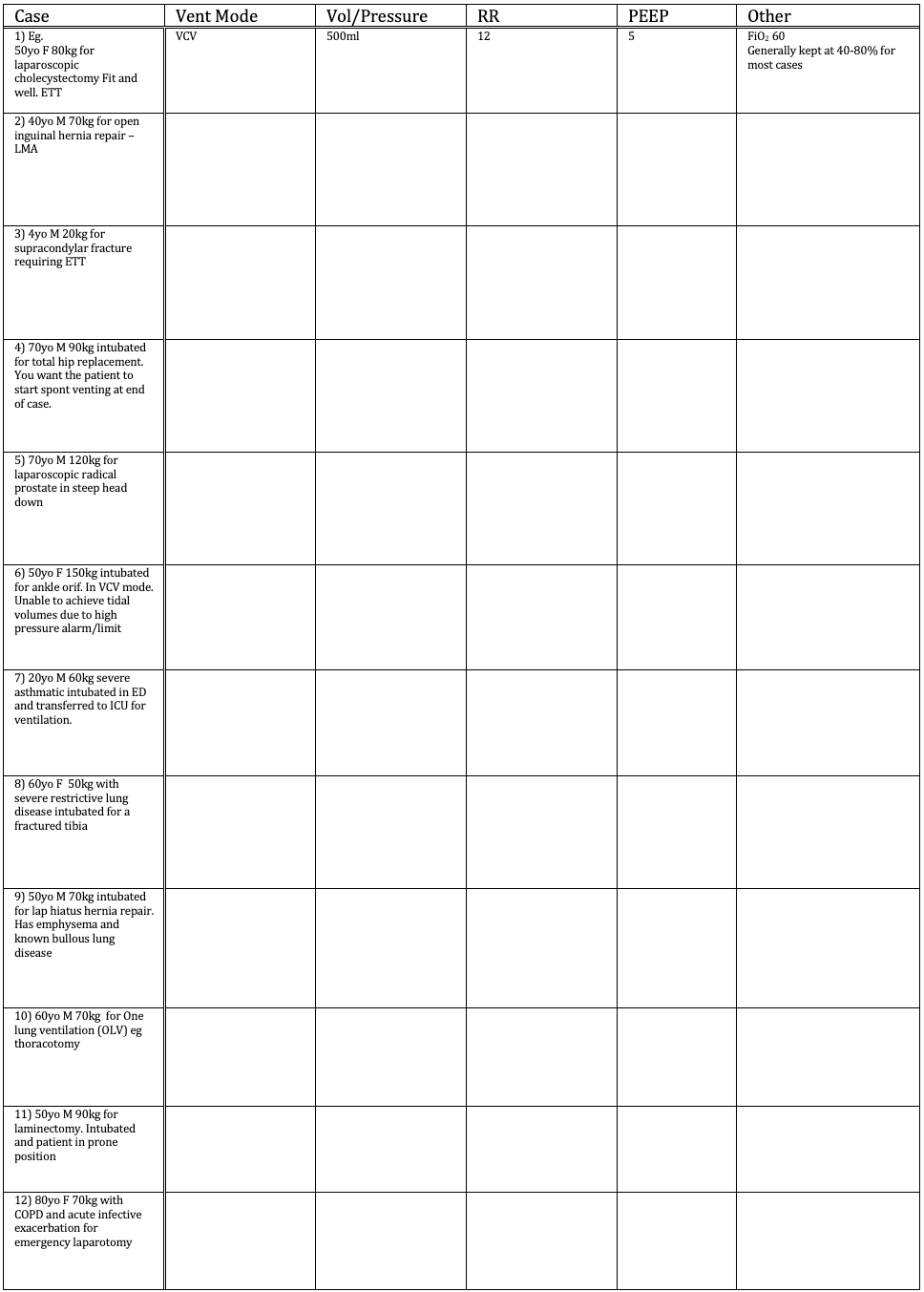
Pressure volume graph
How does mechanical ventilation damage lungs?
- Volutrauma
- Barotrauma
- Atelectrauma
- Infection
How do we minimise damage for sickest lungs? (ARDS)
- Low volume 6ml/kg ventilation (ARDSnet) (↓mortality (31vs40%) and ↑ventilator free days (some evidence in non ARDS lungs)
- Minimise plateau pressure <30cmH2O
- PEEP
- Adv: ↑FRC. ↓collapse and derecruitment. ↓WOB
- Disadv: alveolar overdistension. Deadspace ventilation. Hypotension. ↑ICP
- Ideal PEEP is that which prevents derecruitment and causes minimal overdistension
- Aim at PEEP that gives highest PaO2 and minimum FiO2.
- Practically I check the spirometry loop by pressing the relevant press button on the monitor – and find the PEEP that gives the best compliance.
- Recruitment
- Maintain oxygenation
- Permissive hypercapnoea in sick lungs (eg asthmatics)
- Oxygenation keeps the patient safe
- Most patients will have minimal harm from high CO2.
- Over ventilation of sick lungs may cause more harm
Modes of ventilation
(For GE machines though similar modes will be available on other ventilators)
Select
a) Mode – pressure or volume control
b) RR
c) PEEP
d) Choose amount of pressure support for patient triggered breaths
e) Fine details that I use: IE ratio, max pressure, trigger threshold (ask your consultant and test these)
- Volume control ventilation (VCV)
- Set the volume and RR
- Check pressure limit (autoset to 40cmH2O)
- Constant flow
- Pressure control ventilation (PCV)
- Set pressure and RR
- Constant pressure
- Decreasing flow
- Synchronized intermittent mandatory ventilation (SIMV)
- Choose volume and RR
- Choose pressure support for patient initiated breaths.
- Any patient initiated breaths will either be pressure supported or volume controlled
- SIMV-PC (pressure control)
- Like SIMV except set pressure, RR and pressure support for trigged breaths
- PSVPro (pressure support ventilation Pro)
- Choose pressure support delivered for any patient initiated breaths.
- If long period of apnoea – it will fall to back up mode with SIMV-PC mode with preset settings.
- PCV-VG (pressure control ventilation – volume guaranteed)
- Set volume and RR and PEEP
- The machine will use the lowest pressure to achieve the set VT.
Practical Principles
- Volutrauma seems to be what causes harm in sick lungs so I generally target a maximum volume by using VCV or PCV-VG
- In any circuit with a potential leak (eg. LMA or uncuffed paediatric tubes) part of the target volume may leak out. Therefore I will use pressure targets (PCV or SIMV-PC). This ensures a stable volume is delivered.
- If the high pressures are the limiting factor with ventilation (eg severe asthma or restrictive lung disease) a pressure controlled mode may be the best option to maximise tidal volume and therefore oxygenation.
- At the end of a case when paralysis is not required for anaesthesia or surgery I will change to pressure supported mode eg. SIMV- PSV
This allows one to deliver a set number of breaths while also supporting any patient triggered breaths.
Once the patient is triggering frequent breaths I change to a completely pressure supported mode eg PSVPro or switch to the bagging circuit to allow the patient to breath buy themselves. - Choosing FiO2
- Select <100% oxygen to avoid oxygen toxicity/atelectasis
- Avoid very low FiO2 as there will be minimal reserves if patient extubated risking hypoxaemia
- Most anaesthetists choose somewhere between 40-80% FiO2.
- Consider the risk/benefit of oxygen level for each case* (see cases 11 and 12)*Consider the patient who has a greater chance of dislodgement of ETT.These are often cases where there is a shared airway (ENT/ airway surgery) or surgery where you have limited access to the ETT (prone surgery, large head and neck cases).If the ETT is dislodged then:
If on a lower FiO2, the time to hypoxaemia is shorter
If on a higher FiO2, the patient has greater reserves of oxygen when the ETT is dislodged. Therefore you will have more time to remedy the situation with a decreased risk of hypoxaemia.*Consider a patient whose lungs are prone to worsening hypoxaemia (eg COAD with current infective exacerbation/ asthmatic with an exacerbation/ patient who has aspirated gastric contents on induction)If the patient’s lungs happen to deteriorate then: - If on a higher FiO2, the sats will remain normal in spite of worsening oxygenation.
You will only realize there is a problem when the lungs are so bad that even a high FiO2 is not enough to keep the sats normal.
At this stage you will have no room to increase the FiO2 to keep the patient safe while you assess and treat the problem. - If on a lower FiO2, the sats will fall as the lung condition worsens.
You will realize that something is occurring sooner.
You now have time to keep the patient safe by increasing FiO2, while you assess and treat the problem. - Regular assessments, auscultation and ABGs to calculate Aa gradient will also be valuable during case to assess worsening disease
Step by Step to Ventilator Settings
1. Does patient have airway requiring high pressures to ventilate (asthma, restrictive disease) or is there a leak in the circuit (LMA or uncuffed tube), or are you doing one lung ventilation?
Yes → choose Pressure control mode (PCV)
No → choose volume control mode (VCV)
2. Do you want the patient to eventually breath on their own
Yes → add a pressure support mode eg SIMV if VCV, or SIMV-PC if PCV or PSVPro
3. Tidal volume
- Either dial up 6ml/kg for VCV or choose a pressure that roughly delivers 6ml/kg
4. Respiratory rate
- Generally choose 12 breaths per minute.
- If obstructive lung disease choose lower rate (eg. As low as RR of 4 if severe asthma)
- If restrictive lung disease choose higher rate (eg as high as 20-40 may be required to compensate for very low volumes)
- If you want EtCO2 to increase to encourage spontaneous ventilations, use a lower RR
- Titrate to EtCO2 as required.
5. PEEP
• Generally add 0-10cmH2O of PEEP to maintain lungs at highest compliance
• I use 5cmH2O for most patients
• Choose 0 peep if high pressures limit your ability to deliver a tidal volume (asthma, severe restrictive)
• 5-10 in obese patients to maintain oxygenation and prevent atelectasis
6. FiO2
- Maintain Oxygen sats normal for patient or >94%
- FiO2 60% for most cases
- Is there difficulty accessing your ETT?
Yes → choose higher FiO2 ~ 70-80% - Is there lung pathology that may worsen?
Yes → use lowest FiO2 that safely oxygenates patient (>40% is usually safe)
Examples
What are your ventilator settings for these cases? (Answers on the last page of this PDF document.. don’t look!)