By Zheng Cheng Zhu
Quick Summary
Propofol (2,6-diisopropylphenol) is one of the most widely-used hypnotic agents in critical care departments worldwide, owing to its rapid and predictable onset/offset, favourable safety profile and low adverse effect rates.
However, emerging evidence suggests an association between propofol used in operative and ICU settings and increased mortality.
Most recent meta-analysis of current RCTs by Kotani et al. (2023) highlights a statistically significant 10% increase in mortality in patients undergoing sedation or anaesthesia with propofol versus other agents (RR 1.10, 95%CI 1.01-1.20, p=0.03, I2=0%).
Key subgroups where propofol conferred increased mortality included
- Patients undergoing cardiac surgery vs. any comparator agents (21% increase)
- Volatile anaesthetic as comparator (25% increase)
- Analysis of large RCTs (n>500) (45% increase)
- Studies with low mortality in comparator arm (35% increase)
Four mechanism has been hypothesised explaining propofol’s negative effect on survival
- Propofol infusion syndrome
- Bacterial contamination and infection due to lipophilic medium supporting bacterial growth
- Inferiority compared to, and possible disruption of, organ-protective mechanism of other interventions such as volatile anaesthetic preconditioning
- Intraoperative hypotension secondary to propofol induced vasodilation
Preamble: revision of propofol pharmacology
What is it?
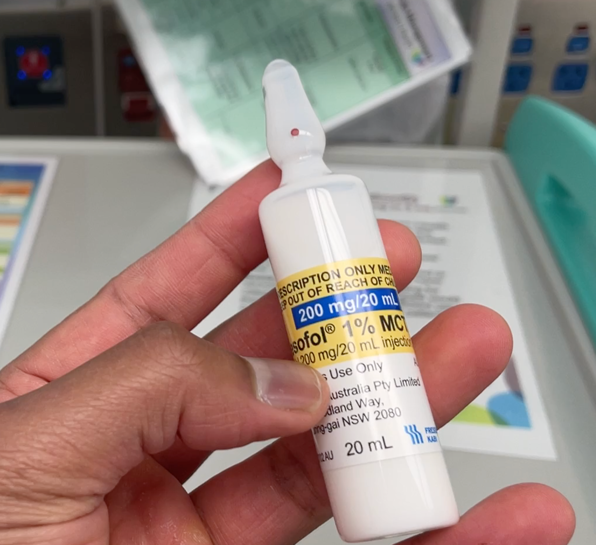
- Chemical structure 2,6-diisopropylphenol
- Intravenous HYPNOTIC AGENT
- Causes sedation, loss of consciousness and amnesia
- DOES NOT HAVE ANALGESIC PROPERTIES
- Due to its low water solubility, it is prepared in mixture of oil emulsion medium, giving its characteristic “milky” appearance:
- 10% soybean oil
- 1.2% purified egg phospholipid
- 2.25% glycerol (for tonicity)
- Sodium hydroxide (for pH control between 6 – 8.5)
- EDTA (antimicrobial additive)
Indications
Anaesthesia
- Induction and maintenance of anaesthesia (total intravenous anaesthesia)
- Sedation
Emergency
- Procedural sedation (usually bolus dosing)
- Rapid sequence induction (can occur in any critical care setting)
ICU
- Maintenance of sedation in mechanically ventilated patients (infusions)
- Neuroprotection (part of multimodal approach) in traumatic brain injury (reduces cerebral metabolism, ICP, cerebral blood flow)
Other
- Off-label use for refractory postoperative nausea and vomiting (antiemetic) and status epilepticus (anti-convulsant)

Pharmacodynamics
- Agonist at beta subunit of CNS γ-aminobutyric acid (GABA)-mediated chloride channels
- Prolongs channel opening, chloride influx, and maintains membrane hyperpolarisation and inhibits postsynaptic neuronal action potential.
Pharmacokinetics
Absorption/administration
- Intravenous administration only
- Not suitable for PO administration due to bitter taste and low oral bioavailability from first pass metabolism (<1%)
Distribution
- Highly protein bound to albumin (predominant) and erythrocyte
- Plasma free fraction 1.2-1.7%
- Highly lipophilic, minimally soluble in water
- Weak acid with pKa 11 = mostly unionised in plasma (pH 7.4) (hence require oil emulsion medium)
- Volume of distribution 2-10L/kg (3-4 times total body volume, despite highly protein bound)
- Readily crosses blood-brain barrier (BBB), free fraction ~31% in CSF
- Rapid onset and offset
- Onset ~30-60s
- Bolus half life ~120s
- Duration of action ~5-10min
- Rapid offset of bolus doses mainly due to rapid redistribution
- Context sensitive half life (time for 50% reduction of plasma drug concentration on STOPPING infusion)
- 10min for 3hr infusion
- 30min for 8hr infusion
- 1-2 days for 10 day infusion (commonly encountered in ICU)
- Half-life INCREASES with prolonged infusion, as more and more drug accumulates in fatty tissue
- Usually not significant in anaesthesia setting
- Half-life to reach steady state: 5-12hrs.
Metabolism
- Mainly hepatic (glucouronide conjugation and hydroxylation)
- Extrahepatic clearance: indicated by clearance rate ~2.2L/min -> higher than liver flow
- Renal and GIT metabolism contributing to extrahepatic clearance
Elimination/excretion
- Renal excretion of inactive metabolites
- Phenolic metabolites rarely (< 1% of patients) result in green discolouration of the urine
Foetal-specific
- Readily crosses the placenta, however rapidly cleared from neonatal circulation
- Non-teratogenic
- Theoretical risk of neonatal respiratory depression
- Induction agent of choice for stable general anaesthesia caesarean sections
Common ADRs
Transient localised pain at injection site
- Offsetted by concurrent IV lidocaine administration
Hypotension
- Indirect effect of sympathetic depression
- Reduced venous vascular tone -> reduced venous return -> reduced preload
- Reduced systemic vascular tone -> reduced total peripheral resistance -> reduced afterload
- Depressed baroreceptor response -> reduced reflex vasoconstriction & tachycardia
- Inotropy is largely unaltered (negative inotropy only at supra-clinical ranges)
- MAP drop largely due to peripheral vasodilation with preserved cardiac output
Respiratory depression
- Dose-dependent dampening of sensitivity to hypoxaemia and hypercarbia, leading to bradypnoea and apnoea
- Attenuated airway reflexes
- Reduced tidal volume via intercostal relaxation
- Bronchodilation (attenuates vagal tone)
Propofol and increased mortality: rationale of meta-analysis by Kotani et al.
Propofol has become a staple in critical care departments in Australia and worldwide, with hundreds and millions of patients each year receiving propofol as their hypnotic agent in theatre, ED departments and ICU. As described it ia an ideal hypnotic with rapid onset, short duration, fast offset and recovery, favourable side effect profile, non-teratogenic and less environmentally harmful compared to volatile gases
With its ubiquitous use presently, any association with worsened survival would have far-reaching ramifications from the sheer number of deaths that may be implicated with the use of propofol.
Kotani and colleagues performed a meta-analysis in 2015 of 133 RCTs, demonstrating a trend towards higher mortality rates with use of propofol compared to other sedation/anaesthesia agents. They postulated 4 mechanisms by which propofol may confer increased harm:
- Propofol infusion syndrome
First described in 1998 in predominantly paediatric ICU populations, it is becoming increasingly recognised in adult ICU patients with prolonged high dose infusion of propofol (greater than 4mg/kg/hr for more than 48 hours), characterised by profound cardiogenic dysfunction and metabolic acidosis.
Incidence
- 1.1%
- 3-4 cases per year for standard ICU
Mortality
- 10-18%
Clinical presentation
- Acute refractory bradycardia leading to asystole and cardiogenic shock
- Preceded by Brugada-like STE in V1-3 and RBBB
- And one or more of:
- HAGMA metabolic acidosis (lactic acidosis)
- Rhabdomyolysis and AKI
- Hypertriglyceridemia
- Hepatomegaly or fatty liver
- And one or more of:
- Mechanism postulated to be inhibition of mitochondrial electron chain reaction, therefore halting muscle aerobic respiration and lipid metabolism
-> anaerobic metabolism predominant -> lactic acidosis
-> cardiac/skeletal muscle lysis, lipidaemia
- Check ABG, UEC, CK, lipid levels and cease propofol infusion immediately with high index of suspicion

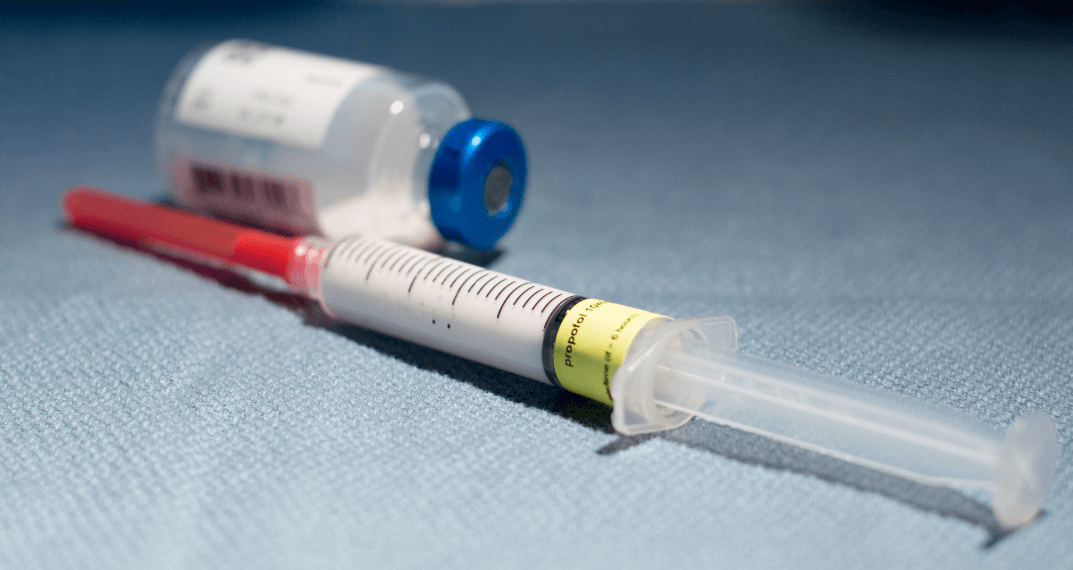
- Iatrogenic Infection
Due to the lipid emulsion preparation, propofol provides an optimal microbial growth environment at room temperature, and hence carries an increased risk of contamination and iatrogenic infection, despite efforts to reduce such risk with the additive EDTA.
In their literature review, Zorilla-Vaza and colleagues identified 20 propofol-related infection outbreaks described between 1989 and 2014 (latest being in Australia, see link: https://www.tga.gov.au/alert/propofol-provive-and-sandoz-propofol-1-emulsion-injection-all-sizes-and-all-batches-update-3), affecting 144 patients and resulting in 10 deaths.
Damningly, poor handling by healthcare professionals accounts for most cases of contamination, some of these described continues to be perpetrated:
- Missed moments of hand hygiene
- Failure to use sterile gloves
- Multiple pre-prepared syringes with prolonged environment exposure
- Inferiority of protective mechanisms compared to other interventions
This relates to propofol’s weaker effect when compared to volatile anaesthetic in preventing ischaemia-reperfusion injury (IRI) in cardiopulmonary bypass and transplant surgery.
In brief, IRI is characterised by mitochondrial respiratory chain dysfunction and uncontrolled production of reactive oxygen species (ROS) after reperfusion of stressed ischaemic tissue, leading to oxidative cell injury, cell apoptosis, pro-inflammatory cell signalling and leukocyte migration.
This translates clinically, in cardiopulmonary bypass, with worsened myocardial infarct and post-operative function; in transplant’s case, this entails delayed graft function and higher rates of primary graft failure.
Preconditioning aims to prime tissue to better tolerate prolonged ischaemic insult during surgery. In this domain, volatile anaesthetics’s pleiotropic effects have been demonstrated to exert cellular protection superior to propofol. Meta-analysis by Bonnani and colleagues (2020) highlighted patients undergoing cardiopulmonary bypass with volatile anaesthetic had reduced myocardial infarct, less inotropic support, better cardiac index and reduced 1-year mortality than those receiving propofol TIVA. Mechanistically, volatiles have been shown to prevent mitochondrial dysfunction by activating protein kinase C, reduce endothelial injury, and upregulation of endogenous hypoxia-protective factors.
In fact, propofol may disrupt these protective mechanisms, by neutralising superoxides and peroxides produced from volatiles implicated in mitochondrial protection.
- Haemodynamic instability
Perhaps one of the better known adverse effects, propofol causes intraoperative hypotension and via sympathetic depression and vasodilation. Combined with critically ill patient populations in ICU (septic, hypovolaemic shock states) and multimorbid surgical candidates with fragile cardiopulmonary reserves, small losses in preload and perfusion pressures often translates to poor survival outcomes.
With further evidence published, Kotani and colleagues have updated their meta-analysis in 2022 to include new RCTs, in hope, with added statistical power, that a clear increase in mortality with propofol compared to other comparactors can be elucidated.
Study design
PICO question
- Population: patients receiving general anaesthesia or sedation
- Intervention: propofol
- Comparison: any comparator drug
- Outcome: mortality at the longest follow-up available
Search method
- 4 investigators
- Database:
- Pubmed, Google Scholar, Cochrane Central Register of Controlled Trials, ClinicalTrials.gov
- Abstracts of major congresses within last 3 years
Inclusion
- All RCTs comparing propofol vs. any comparator in any clinical setting
- All age, all language
Exclusion
- Cross-over trials
- Non-human studies
- Comparators were loco-regional anaesthesia
- Indication for palliative / end-of-life care
- Propofol used as single bolus in intervention arm, or simple procedures
Study selection / data collection / risk of bias
- 2 investigators selected eligible studies, disagreement discussed with 2 senior investigators
- 2 investigators extracted data: publication details, n (propofol), n (comparator), comparator type, no. deaths, settings (ICU / surgery (non-cardiac vs cardiac) / adult vs. paediatric)
- Risk of bias was assessed with Cochrane risk-of-bias tool ver. 2 (RoB 2 )
Data analysis
- Relative risk (RR) calculated from:
- Fixed-effect Mantel-Haenszel model for low heterogeneity (I2<25%)
- Random-effect Mantel Haenszel model for high heterogeneity (I2≥25%)
- Standard two tailed 0.05 significance level for unadjusted p values
- Prespecified subgroup analysis
- Settings: Cardiac / non-cardiac / ICU
- Bolus propofol in comparator arm: yes / no
- Sensitivity analysis subgroups
- Age: adult / paediatric
- Comparator type: volatile, total IV, miscellaneous
- Study size: large (n≥500) / small (n<500)
- Comparator mortality: high (>4.5%), low (≤4.5%)
- Exclusion of high bias risk studies
- RR and 95% confidence interval (95% CI) plotted on probability density function (100,000 simulated trials on log scale using kernel density estimation)
- Post-hoc sensitivity analysis with Bayesian meta-analysis and trial sequential analysis (TSA)

Outcome
252 RCTs were selected for analysis, with 30,757 total patients.
- Most common setting was non-cardiac surgery (153 RCTs) > ICU (52 RCTs) > cardiac surgery (47 RCTs).
- Most common comparator was volatile anaesthetics (172 RCTs), followed by total IV agents other than propofol (71 RCTs) and miscellaneous (9 RCTs)
- 75 RCTs included propofol bolus in their comparator arm (for anaesthesia induction)
Bias assessments:
RoB2 identified 41 high risk studies (16%), 114 moderate risk (45%) and 97 low risk (38%).
Funnel plot showed no obvious asymmetry to suggest publication bias.
Bubble plot did not show influence of year of publication on mortality ratio.
Primary outcome: Morality
Analysis demonstrated a statistically significant 10% increase with use of propofol
- 5.2% propofol vs. 4.3% comparator, RR 1.10, 95% CI 1.01–1.20, p = 0.03, I2=0%
- Probability density function with Bayesian meta-analysis confirms a 98.4% probability of increase in mortality
- TSA fell in “inconclusive” range, Z-line favouring “comparator” but not crossing into significance range
Subgroup analysis
Significant mortality increase with propofol were noted in:
- Patients undergoing cardiac surgery vs. any comparator (21% increase)
- RR 1.21, 95%CI 1.04-1.41, p=0.01, I2=0%
- Volatile anaesthetic as comparator (25% increase)
- RR 1.25, 95%CI 1.06-1.47, p=0.009, I2=11%
- Analysis of large RCTs (n>500) (45% increase)
- RR 1.45, 95%CI 1.10-1.92, p=0.009, I2=0%
- Studies with low mortality in comparator arm (35% increase)
- RR 1.35, 95%CI 1.03-1.76, p=0.03, I2=0%
Overall significance was retained after removing high risk RCTs based on RoB2
- RR 1.12, 95% CI 1.02-1.23, p=0.02, I2=0%
Of note, propofol’s use in non-cardiac surgery and ICU setting were not associated with significant increase in mortality compared to comparators.
This was also the case irrespective of whether propofol was used for bolusing in the comparator arm.
Implications of current meta-analysis
Kotani and colleagues have shown that propofol, one of the most commonly used medications in any anaesthetist’s trolley, is associated with a 10% increase in mortality compared to other hypnotics.
Not unexpectedly, this meta-analysis has shown that propofol is worse than volatile anaesthetics, particularly in cardiac surgery. This brings more credibility to the hypothesis that propofol offsets the organ-conditioning effects of volatile anaesthetics and leads to greater IRI in cardiac surgeries, where cardiopulmonary and renal circulations are often subjected to prolonged ischaemia and sudden reperfusion. It would also be remiss to discount the detrimental haemodynamic effects of propofol in such high-risk surgery types.
We may infer that propofol infusion syndrome is unlikely to play a major role in mediating increased mortality. As a syndrome most commonly observed in paediatric populations subjected to prolonged propofol infusion, neither the ICU nor paediatric subgroups saw significant risk increases.
Infection risk of propofol leading to worsen mortality rates is difficult to extrapolate. Data continues to observe significant increases in mortality when investigating RCTs published post-2005 (RR 1.11, 95% CI 1.00-1.22, p=0.04, I2=0%), a timeframe after the widespread adoption of EDTA as an antimicrobial additive in propofol preparation. As described, poor handling and preparation techniques remain preventable sources of microbial contamination and harm to patients. Whether this risk is independently observed is up for further debate, amidst an increasingly complex and at-risk surgical population under an environment with ever-evolving antibiotic resistance patterns.
In the ICU setting, propofol’s negative effect, if any, appears to be less overt. The authors highlighted the heterogeneity of the ICU population requiring sedation in terms of their presenting pathologies and background co-morbidities, making propofol effects difficult to discern from confounding noise. High baseline mortality rates of ICU patients also makes detecting any treatment effects of propofol challenging, as demonstrated in the statistical non-significance of the “high-mortality comparator arm” subgroup.
Nevertheless, it is important to note that all subgroups, irrespective of statistical significance, had effect sizes in favour of propofol reducing survival. Kotani and colleagues affirmed the robustness of the outcomes with a consistent Bayesian post-hoc meta-analysis.
However, the data at hand does highlight some limitations to our interpretations.
- Substantial proportion of studies included propofol in the comparator arm (as part of induction protocol), which may undermine the legitimacy of the supposed “control” group
- The TSA finding was “inconclusive”, implying that additional data from future studies has the potential to unmask and correct any Type I error within the current RCT pool.

What does our finding imply? Assuming millions of patients worldwide receive propofol annually, this implies an unacceptably high mortality burden that the critical care specialties are subjecting our patients to.
Will this meta-analysis inform clinical change at present? Very unlikely, given the lack of large megatrials informing this meta-analysis, contamination of propofol in the comparator arm, as well as our clinical inertia ingrained in our practice guidelines and the financial implications. However, it is likely to provoke a consideration of a large trial, which will be a resource-intensive undertaking.
References
Kotani, Y., Pruna, A., Turi, S. et al. Propofol and survival: an updated meta-analysis of randomized clinical trials. Crit Care 27, 139 (2023). https://doi.org/10.1186/s13054-023-04431-8
De Cassai, A., Tassone, M., Geraldini, F., Sergi, M., Sella, N., Boscolo, A., & Munari, M. (2021). Explanation of trial sequential analysis: using a post-hoc analysis of meta-analyses published in Korean Journal of Anesthesiology. Korean journal of anesthesiology, 74(5), 383–393. https://doi.org/10.4097/kja.21218
Folino TB, Muco E, Safadi AO, et al. Propofol. [Updated 2022 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430884/
Nieuwenhuijs-Moeke, G. J., Bosch, D. J., & Leuvenink, H. G. D. (2021). Molecular Aspects of Volatile Anesthetic-Induced Organ Protection and Its Potential in Kidney Transplantation. International journal of molecular sciences, 22(5), 2727. https://doi.org/10.3390/ijms22052727
Sahinovic, M. M., Struys, M. M. R. F., & Absalom, A. R. (2018). Clinical Pharmacokinetics and Pharmacodynamics of Propofol. Clinical pharmacokinetics, 57(12), 1539–1558. https://doi.org/10.1007/s40262-018-0672-3
Yartsef, A (2015), Propofol. CICM Primary Exam. Deranged Physiology. Last accessed 24/04/2023. Available from: https://derangedphysiology.com/main/cicm-primary-exam/required-reading/nervous-system/Chapter%20211/propofol
Zorrilla-Vaca, A., Arevalo, J. J., Escandón-Vargas, K., Soltanifar, D., & Mirski, M. A. (2016). Infectious Disease Risk Associated with Contaminated Propofol Anesthesia, 1989-2014(1). Emerging infectious diseases, 22(6), 981–992. https://doi.org/10.3201/eid2206.150376