The PADDI trial
by Dr. Matthew Vella @mjv.igee
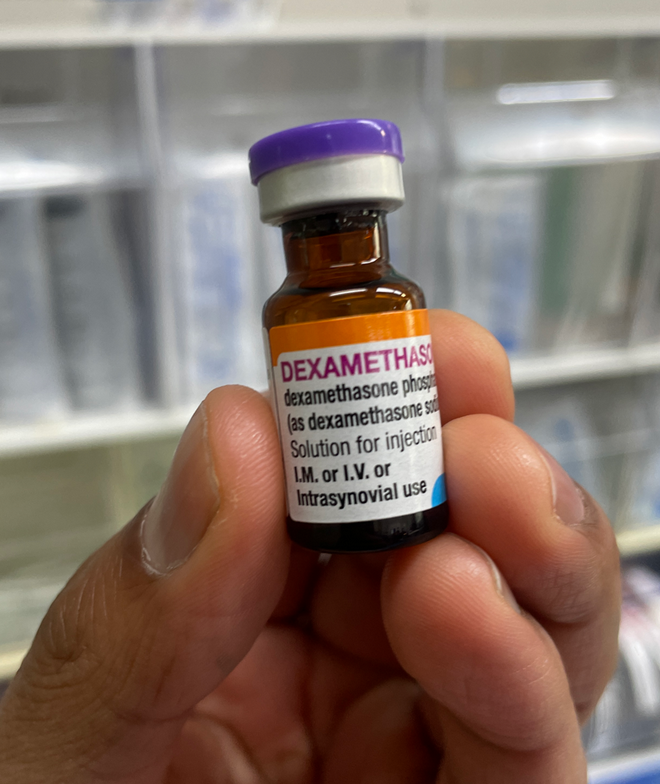
PADDI (The Perioperative ADministration of Dexamethasone and Infection Trial)
Corcoran, T. B., Myles, P. S., Forbes, A. B., Cheng, A. C., Bach, L. A., O’Loughlin, E., Leslie, K., Chan, M. T. V., Story, D., Short, T. G., Martin, C., Coutts, P., Ho, K. M., PADDI Investigators, Australian and New Zealand College of Anaesthetists Clinical Trials Network, & Australasian Society for Infectious Diseases Clinical Research Network (2021). Dexamethasone and Surgical-Site Infection. The New England journal of medicine, 384(18), 1731–1741. https://doi.org/10.1056/NEJMoa2028982
Where is it published?
New England Journal of Medicine (NEJM)
What kind of study is it?
International, multi-centre, randomised, placebo controlled, triple blind, non-inferiority trial
Who is involved?
ANZCA (Australian and New Zealand College of Anaesthetists) Clinical Trials network
Australasian Society for Infectious Diseases Clinical Research Network
Centres across Australia, Hong Kong, China, New Zealand and South Africa
What did they set out to do?
To see if intraoperative dexamethasone is associated with increased rates of surgical site infection

What is significant about the study?
It explores whether we have been exposing patients to greater risk of surgical site infection by providing PONV prophylaxis
This time we’re looking at a higher, single intraoperative dose (8mg) compared with previous studies [e.g., 4mg single dose in Kurz et al (2015); 14mg tapered over 3 days in Abdelmalak et al (2013)]
How was it done?
Many adults, from centres across the globe, with ASA scores 1-4 (American Society of Anaestheiology), were randomly allocated to receive dexamethasone (8mg intravenous) or placebo during GA (general anaesthesia) for elective non-cardiac surgery
Patients with diabetes were included (Hba1c <9), however those receiving surgery for a primary infection were excluded. All other anaesthetic care was provided according to local practice / guidelines (including antibiotic provision and BGL management)
See full list of inclusions / exclusions:
https://bmjopen.bmj.com/content/9/9/e030402.long
Patients were followed-up in PACU (post acute care unit), with post-op wound reviews on day 1, 3, discharge, 30-days, and 6-months
The primary outcome was the occurrence of surgical site infection within 30-days
Why do we care about dexamethasone use?
PONV remains a major challenge in perioperative care. Around 1 in 4 people will experience PONV after general anaesthesia, and this rate jumps to around 3 in 4 in high-risk populations (i.e., younger, female, previous PONV, history of motion sickness, non-smoker, post-op opioid usage)
While dexamethasone is a potent, prophylactic anti-emetic, we know that long-term glucocorticoid therapy is associated with increased risk of surgical site infection and wound dihescence
In short, we want to ensure our effort to minimise PONV – with the aim to improve patient experience / care, length-of-stay, mortality and morbidity, and associated healthcare costs – is not subjecting patients to greater risk of surgical site infection

What did they find?
We’re doing the right thing by the patient!
There was no difference between dexamethasome and placebo in incidence of surgical site infection within 30 days of non-urgent, non-cardiac surgery
Dexa, diabetics and other at-risk patients
There was not an increased incidence of surgical site infection in diabetics or at-risk patients – in fact, dexamethasone was equal to placebo across all subroups and is considered safe for patients with implanted prosthetic material
Any limitations?
1. No pre-trial data collected on baseline patient risk-factors (e.g., subtype of GI surgery, pre-op bowel or skin preparation, antibiotic prophylaxis duration / schedule)
2. Potential for mild infections to be missed due to failed follow-up (i.e., patient not returning)
3. Issues with non-adherence to protocol (i.e., non-trial provision of post-op glucose)

What’s the overall take-home?
Dexamethasone can be used safely and effectively for PONV prophylaxis without fear of exposing patients to increased risk of surgical site infection.
Importantly, the PADDI trial suggests our total knee replacement case with diabetes and a history of severe PONV can have dexamethasone providing they have a reasonable pre-operative BGL control (i.e., Hba1c <9).
Further reading:
PADDI trial: rationale and design
https://bmjopen.bmj.com/content/9/9/e030402.long
PADDI trial results webinar
https://www.youtube.com/watch?v=-XdkpDmD1rM
CDC – centers for disease control and prevention: surgical site infection guideline
https://www.cdc.gov/infectioncontrol/guidelines/ssi/index.html
Previous studies with lower / tapered dose of dexamethasone:
Abdelmalak, B. B., Bonilla, A., Mascha, E. J., Maheshwari, A., Tang, W. H., You, J., Ramachandran, M., Kirkova, Y., Clair, D., Walsh, R. M., Kurz, A., & Sessler, D. I. (2013). Dexamethasone, light anaesthesia, and tight glucose control (DeLiT) randomized controlled trial. British journal of anaesthesia, 111(2), 209–221.
A. Kurz, E. Fleischmann, D. I. Sessler, D. J. Buggy, C. Apfel, O. Akça, the Factorial Trial Investigators, Edith Fleischmann, Erol Erdik, Klaus Eredics, Barbara Kabon, Friedrich Herbst, Sara Kazerounian, Andre Kugener, Corinna Marschalek, Pia Mikocki, Monika Niedermayer, Eva Obewegeser, Ina Ratzenboeck, Romana Rozum, Sonja Sindhuber, Katja Schlemitz, Karl Schebesta, Anton Stift, Andrea Kurz, Daniel I. Sessler, Endrit Bala, Samuel T. Chen, Jagan Devarajan, Ankit Maheshwari, Ramatia Mahboobi, Edward Mascha, Hassan Nagem, Suman Rajogopalan, Luke Reynolds, Adrian Alvarez, Luca Stocchi, Anthony G. Doufas, Raghavendra Govinda, Yusuke Kasuya, Ryu Komatsu, Rainer Lenhardt, Mukadder Orhan-Sungur, Papiya Sengupta, Anupama Wadhwa, Susan Galandiuk, Donal Buggy, Mujeeb Arain, Siun Burke, Barry McGuire, Jackie Ragheb, Akikio Taguchi, the Factorial Trial Investigators, Effects of supplemental oxygen and dexamethasone on surgical site infection: a factorial randomized trial, BJA: British Journal of Anaesthesia, Volume 115, Issue 3, September 2015, Pages 434–443