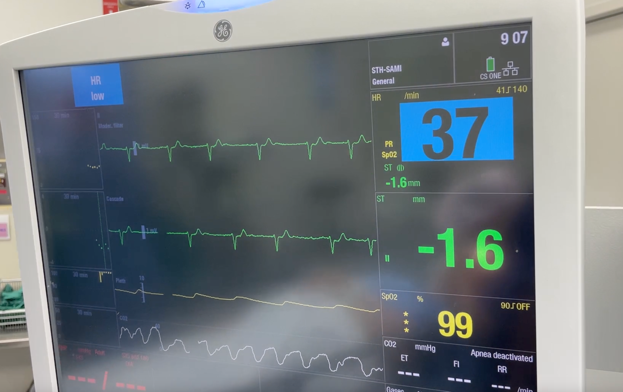
Bradycardia is defined as a heart rate below 60bpm and occurs commonly under anaesthesia. Although most bradycardias are benign, they have the potential to cause haemodynamic compromise and progress to asystole/cardiac arrest. Being able to predict when a bradycardia may occur, as well as understanding the underlying cause, is pivotal to early and successful treatment.
General approach to the management of bradycardias
SAFETY
- Confirm reading
- Call for help (depending on severity / seniority)
- Scan patient / surgical field / anaesthetic / monitors (check oximeter and capnography to rule out hypoxaemia; assess ECG for 2nd or 3rd degree blocks)
- Stop surgery / remove stimulus (eg, pneumoperitoneum, pressure on globe, squint surgery, spermatic cord manipulation)
TEMPORISATION / INITIAL MANAGEMENT
- Administer IV atropine 300-600mcg boluses to a maximum of 3mg (IV glycopyrrolate 200-400mcg boluses may also be considered depending if less severe bradycardia)
- Consider IV ephedrine 3-12mg boluses if hypotension and bradycardia present despite administration of anticholinergic
- IV fluids and legs up / Trendelenburg position to optimise preload and venous return to heart (underfilled heart may cause a Bezold Jarisch reflex causing bradycardia)
- IF ABOVE FAILS
- Administer 100% oxygen and ensure airway is safe/managed with basic to advanced techniques.
- Early preparation of transcutaneous pacing, especially if 2nd or 3rd degree block present on rhythm strip
- IV adrenaline at 10-100mcg boluses (while awaiting pacing) If responsive, consider adrenaline infusion at 0.05-0.10 mcg/kg/min
- IF ASYSTOLE/ARRREST
- Commence CPR with advanced life support algorithm
DIAGNOSIS
- Probability gambit – See below for common causes of bradycardias during anaesthesia (surgical / anaesthetic causes)
- 4 H’s and 4 T’s
- Underlying cardiac pathology – 12 lead ECG, ECHO, bloods, and cardiology consult.
Common causes of bradycardia during anaesthesia
Bezold-Jarisch reflex
- Common cause – Following spinal anaesthesia or as a complication of an interscalene brachial plexus block, pneumoperitoneum.
- Trigger – Ventricular chemoreceptors and mechanoreceptors are stimulated by reduced ventricular filling, chemical substances, or drugs.
- Response – Increased renin and vasopressin release, sympathetic nervous system (SNS) inhibition and parasympathetic nervous system (PNS) activation.
- Initial treatment –
- Cease trigger (deflate pneumoperitoneum)
- Administer atropine (300-600mcg) and
- increase preload (IV fluid / Trendelenburg / legs up).
- Other medications may be required (ephedrine, adrenaline)
- If severe bradycardia or asystole – commence ALS measures
Oculocardiac reflex
- Common cause – Facial or ocular surgery, where the trigeminal nerve may be involved.
- Trigger – Direct pressure placed on the extraocular muscles, globe, or conjunctiva mediates reflex through connections between the ophthalmic branch of the trigeminal nerve and the vagus nerve.
- Response – PNS activation.
- Initial treatment –
- Remove pressure from area.
- Administer atropine (300-600mcg) or glycopyrrolate (200-400mcg).
Bradycardia due to pneumoperitoneum
- Common cause – Laparoscopic surgery.
- Trigger – Peritoneal stretch due to CO2 insufflation of the peritoneum during laparoscopic surgery.
- Response – SNS inhibition and PNS activation.
- Initial treatment –
- Pneumoperitoneum deflation and stop surgery.
- Administer atropine (300-600mcg) or glycopyrrolate (200-400mcg).
- Other medications may be required (ephedrine, adrenaline)
- If severe bradycardia or asystole – commence ALS measures
Bradycardia due to spermatic cord traction
- Common cause – Orchidectomy or inguinal hernia repair where there is manipulation of the spermatic cord.
- Trigger – Manipulation/traction on spermatic cord results in vagal reflex.
- Response – SNS inhibition and PNS activation.
- Initial treatment –
- Release traction on spermatic cord.
- Administer atropine (300-600mcg) or glycopyrrolate (200-400mcg).
Bradycardia due to endotracheal suctioning
- Common cause – Endotracheal suctioning in mechanically ventilated patients.
- Trigger – Vagus nerve stimulation.
- Response – PNS activation.
- Initial treatment –
- Stop suctioning,
- 100% O2. Atropine (300-600mcg) or glycopyrrolate (200-400mcg).
Bradycardia due to suxamethonium
- Common cause – Administration of suxamethonium in a young patient, particularly when a second dose is given.
- Trigger – Activation of nicotinic receptors causes muscarinic stimulation resulting in bradycardia.
- Response – Increased vagal tone.
- Initial treatment –
- Administer atropine (300-600mcg)
- Anticholinergics may be considered as pre-treatment in patients of higher risk (eg, paediatric patients).
Bradycardia due to metaraminol
- Common cause – Administration of metaraminol.
- Trigger – Increased arterial pressure in response to vasoconstriction is detected by baroreceptors (baroreceptor mediated reflex).
- Response – SNS inhibition and PNS activation.
- Initial treatment –
- Often no treatment required, but may exacerbate other causes of bradycardia
- Eg giving metaraminol for a low BP, as pneumoperitoneum is being commenced.
- Administer atropine (300-600mcg) or glycopyrrolate (200-400mcg).
- Other medications may be required (ephedrine, adrenaline)
- If severe bradycardia or asystole – commence ALS measures
- Often no treatment required, but may exacerbate other causes of bradycardia