An 80kg 50yo male enters theatre directly from the emergency department for an urgent laparotomy. He has been involved in a motor vehicle accident and is thought to have lost up to 4L of blood. Despite valiant efforts at resuscitation, you know that he is still significantly unstable and under volume.
What dose of propofol you administer for your rapid sequence induction?
This is an incredibly high risk induction with a chance of the patient arresting on the table. They are many ways to do a cardiostable induction for this patient, and they all require lower doses of hypnotic with careful titration, a rapid acting muscle relaxant (suxamethonium or 1.2mg/kg of rocuronium) and concurrent administration of a vasopressor (metaraminol) to maintain preload and afterload.
Depending on how dire the situation is, I may only give 10-50mg of propofol due to the devasting hypotension it may cause in this patient.
Compare this with the 150-200mg of propofol I may administer if this same patient was to be induced for an elective laparoscopic cholecystectomy.
NB there are many other safe ways to induce this patient using cardiostable medications like ketamine, etomidate and midazolam, combined with opioids. however propofol at the correct dose and method is a commonly used technique.
The following summarises the pharmacology and physiology with respect to propofol inductions.
Propofol has been widely recognised for its analgesic, hypnotic, and haemodynamic effects. However, unlike the first two factors, the latter is much less established in terms of a dose-response relationship, often accepted as an inevitable side effect of propofol.
This study creates empirical models for the effect of propofol on mean arterial pressure (MAP), heart rate (HR), and stroke volume (SV). *SV was approximated by pulse pressure
So why is this important?
Evidence suggests that hypotension during general anaesthesia is associated with perioperative and postoperative mortality. Hence, having a calculable risk may facilitate the optimisation of propofol use in patients where hypotension is particularly dangerous.
How does propofol induce haemodynamic instability?
According to this study, the haemodynamic parameters most affected by propofol infusion were MAP, total peripheral resistance (TPR), SV, and HR (inversely to TPR). Specifically, TPR and SV decreased most significantly. The estimated 50% concentrations of propofol required to elicit changes in TPR and SV were 2.96 and 0.34 μg ml−1 respectively. TPR reduced more so than SV, with max propofol-induced changes being -85.1% and -23.5% respectively.
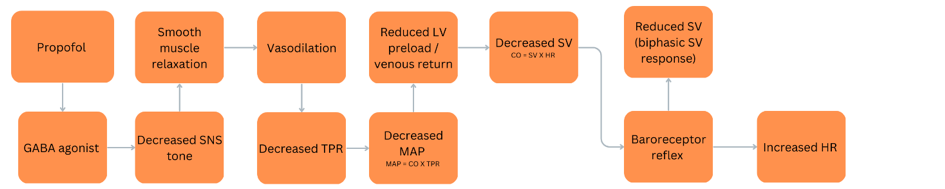
- Propofol is a positive modulator of y-aminobutyric acid (GABA) receptors leading to a decrease in sympathetic (SNS) tone.
- This results in vasodilation by relaxation of smooth muscle and a reduction TPR, and hence MAP. (MAP = CO X TPR = HR X SV X TPR)
- A reduction in MAP reduces LV preload and hence SV.
- Negative feedback from the baroreceptor reflex results in increased HR, and later SV. Causing a biphasic effect in SV during propofol infusion – an initial decrease and subsequent proportional increase in SV with increasing time and concentration.
Are there any anomalies to this?
The negative feedback to increase HR seen in this study is particularly notable. Propofol has previously been thought to inhibit this rebound tachycardia by inhibiting the baroreceptor reflex. This phenomenon requires further investigation.
Further, SV was more affected in older volunteers. The max effect in older volunteers (e.g. 85 years old) was predicted to be -86.2%, compared with -23.5% in younger individuals (e.g. 35 years old). Consequentially, the equations established by this study showed that MAP and HR were also affected to a larger extent in older volunteers.
Reference