How to increase your learning curve when there are limited learning opportunities
It seems that regional anaesthesia is somewhat past its heyday.
Many hospitals have adopted other techniques for pain management in operations that were once common practice grounds for regional, hospitals don’t have the systems set up to facilitate fast turnover and having sufficient time for regional anaesthesia onset and there are no studies to prove convincingly any long term morbidity or mortality benefit.
However in my experience this is one of the most incredibly useful skills in your anaesthesia quiver!
There will be many times in your career that you will be required to anaesthetise an incredibly sick patient for a peripheral/limb procedure.
Imagine a patient from ICU requiring an urgent open reduction and fixation of his fractured ankle. He is 150kg, on BIPAP for pneumonia, heart failure with EF30% and saturating at 90% due to his severe COPD. Performing a general anaesthetic for this operation is definitely an option and will require a lot of prep time and may result in airway management difficulty, CVS instability and oxygenation risks. And this situation isn’t that uncommon! It will arise time and time again whether it’s an upper limb procedure, lower limb procedure or the elective arterio-venous fistula in a sick renal patient.
I would argue your ability to perform effective regional anaesthesia improves welfare for the patient and ease of providing effective anaesthesia for you and your team!
So with fewer opportunities to provide regional anaesthesia how do you gain enough experience? If practice makes perfect how do you get enough practice?
It is vital to manufacture practice and create opportunities!
What do I mean? Well there are a few select skills with ultrasound (US) guided regional anaesthesia that you can master even with minimal practice at actual regional anaesthesia. ‘Chunking’ these skills and practising them separately is one of the best ways to learn difficult and uncommon techniques
These skills are:
- US scanner competence
- Sono-anatomy mastery
- US-Needle coordination
US scanner competence
- Bring out the US scanner at every opportunity to scan nerves, veins, arteries and hearts
- Learn a systematic way of improving your image.
- Select the correct probe
- Select the depth
- Optimise the gain (how much signal or ‘whiteness’ comes back)
- Select the focal point
- Probe manipulation: practice sliding, tilting, rotating and translating
Sono-anatomy mastery
Sono-anatomy is like exploring a new neighbourhood. The first few times everything is unfamiliar and you won’t recognise much. You then decide to buy a map and explore your new neighbourhood every day and suddenly you will start to recognise signs, roads, laneways and your favourite cafes and shops.
The way I increased my familiarity with the sonoanatomy neighbourhood was to scan a patient every day. My map was Ultrasound Imaging for Regional Anaesthesia from www.usra.ca/education/booklet.php (electronic copy available on iTunes). This is an exceptional resource, which shows the labelled cadaveric and sono-anatomy so you can trace the nerves from proximal to distal in the upper and lower limb.
Put a probe on the consented patient and try the following. For your lower body cases try tracing the brachial plexus from the interscalene, to supraclavicular, infraclavicular and axillary views and then trace the terminal nerves (ulnar, median and radial) from axilla to the wrist. Likewise during your upper body cases you can ‘walk’ around the lower limb sono-anatomy neighbourhood tracing the femoral nerve and sciatic nerves. Use Ultrasound Imaging for Regional Anaesthesia to show you the relevant structures.
After doing this a few times you will gain familiarity of the
- nerve plexuses
- nearby structures,
- the way nerves often follow vascular structures and
- the way they differ from tendons and muscles.
- With even more experience you will notice the inter-patient variability and abnormal anatomy. This becomes increasingly relevant when you notice that some patients are difficult to block because they have aberrant nerves, tissue/septae that divide plexuses or vascular structures running nearby.
Another great way to have guided practice is to sign up to one of the many US regional anesthesia short courses.
Other useful resources include:
- www.nysora.com
- www.asra.com
- AnSo app

US needle coordination
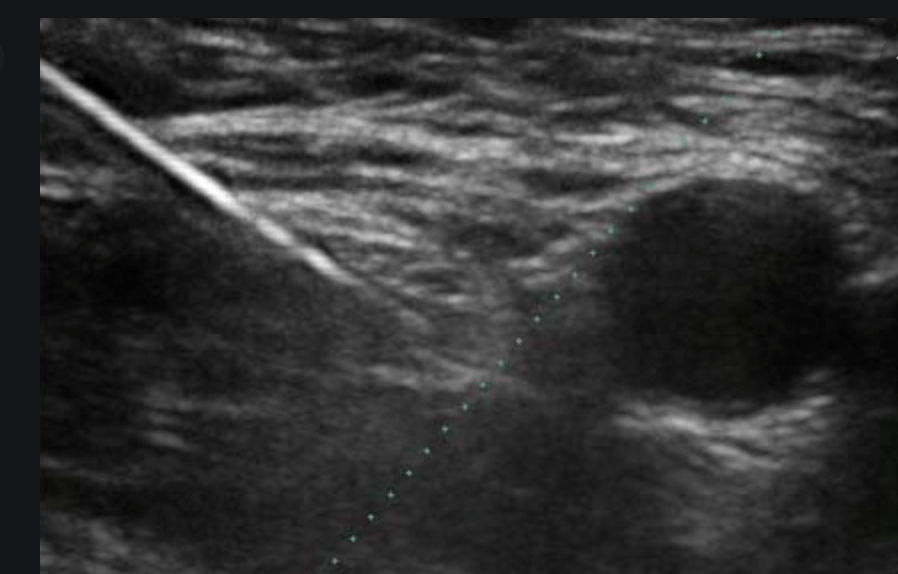
There are many techniques that are common in anaesthesia and enable us to practice US needle coordination. After you have mastered cannulation try performing cannulation with US guidance. This is a great way to improve your success with difficult cannulation but also a great way to learn how to coordinate your needle manipulation in one hand and the US probe in the other.
Other slightly advanced techniques to improve US coordination are US guided arterial line insertion and central line insertion.
In my experience there were some relatively common opportunities for US guided regional anaesthesia. The fascia iliaca blockand femoral nerve blockare considered relatively safe and easy techniques and where I developed most of my skills in US coordination. They are superficial, the landmarks are easy to find, have few critical structues and inadvertent vascular puncture can be compressed to stop a haematoma. When clinically indicated, do these regional blocks with US guidance.
So there is it! My method for trying to increase your learning curve, when your learning opportunities might be few and far between.
Any questions or comments please email me
Anaesthesiacollective@gmail.com