by Dr. Matthew Vella
@mjv.igee
#Anaesthesia #anaesthetics #anesthesiology #anesthesia #anesthetic #abcsofanaesthesia #medicine #anesthesiologist #anaesthetist #anesthetist #anaesthesiology #nurse #medical #meded #FOAMed #medicalstudent #geriatrics #trauma #hipfracture #NOF
Title:
Guideline for the management of hip fractures 2020
Griffiths, R., Babu, S., Dixon, P., Freeman, N., Hurford, D., Kelleher, E., Moppett, I., Ray, D., Sahota, O., Shields, M., & White, S. (2021). Guideline for the management of hip fractures 2020: Guideline by the Association of Anaesthetists. Anaesthesia, 76(2), 225–237. https://doi.org/10.1111/anae.15291
Journal:
Anaesthesia (Association of Anaesthetists, United Kingdom)
Author(s):
A multidisciplinary ‘Working Party’ on behalf of the Association of Anaesthetists
Aim:
To update Hip Fracture Management Guidelines – considering new evidence and consensus established since the previous guide in 2011
To encourage standardisation of anaesthetic management and multidisciplinary care in line with current consensus / guidance

Significance:
The guideline directs perioperative hip fracture management, covering:
(i) core aims and principles of perioperative management
(ii) acknowledgement of the wider role of anaesthetists in perioperative care
(iii) specific changes to the 2011 guideline
(iv) areas of controversy
(iv) links to important supplementary material
How it was done:
The multidisciplinary Working Party – consisting of contributors from across a range of hospital departments in the United Kingdom – builds on the 2011 guideline to comment on interim developments in evidence and consensus gleaned from research, audit, guidelines, databases and scoring tools (e.g., UK national hip fracture databases, Fragility Fracture Network Guideline, Hip Fracture Perioperative Network, Nottingham Hip Fracture Score).
Notable mention:
It has been worth it!
Since release of the 2011 guideline, there has been significant improvements in key areas including: time to orthogeriatric assessment, time to operation, time to remobilisation, length of stay, and a reduced burden on individuals (i.e., patient and family) and public healthcare (i.e., national health service finances).
Overall, the 30-day mortality post hip fracture surgery in England and Wales decreased from 10.9% (2007) to 6.1% (2018).
Framework:
The Working Party lists the aims of hip fracture management and how they’re linked to anaesthetic care (i.e., pain, nausea and vomiting, delirium, constipation)
- Preoperative preparation
- promptly to theatre (< 36 hours), analgesia (i.e., nerve blocks), fluids, multidisciplinary care
- Remobilisation
- as per NICE guideline, and aiming within the first 24-hours post-op
- Re-enablement
- aim within 2-5 days post-op
- Rehabilitation
- long-term aim, and delays may be traced to complications in preceding steps
Type of anaesthesia:
- Spinal vs General Anaesthesia
- the adoption of standardised anaesthetic care is likely attributable to a lack of new / focused research
- effects related to anaesthesia are small relative to the effects of trauma, surgery, orthogeriatric care and individual patient factors (e.g., age, frailty, cognitive impairment)
- consider careful delivery more than the type of anaesthesia
- individual hospitals should develop standards based on consensus achieved through multidisciplinary approach
- focus on improving the predictability around technique so its post-op complications may be better anticipated and managed (i.e., by allied health staff) as the patient progresses through remobilisation, re-enablement and rehabilitation
- ongoing quality assurance and quality improvement remain vitally important

Key changes since 2011: (Working Party recommendations / comments)
- Analgesia
- Provide femoral or fascia iliaca nerve block in ED and at time of surgery (allowing 6-hours)
- Aim for ultra-sound guided placement to improve adequacy
- Routine peripheral nerve blockade supplements general or spinal anaesthesia (i.e., reduces need for additional sedation or IV analgesia)
- Reserve the use of high volume, low concentration pericapsular/periosteal injection for posterior surgical approach (i.e., when blocking lateral cutaneous nerve of thigh won’t work)
- Deprivation of liberty standards
- Be aware that our actions may deprive patients of their liberties (i.e., liberal use of intraoperative sedation / IV analgesia may increase the risk of post-operative delirium and thus the provision of chemical and/or mechanical restraints)
- Goals of Care / Advanced Care Directives
- Confirm / record resuscitation status prior to commencing anaesthesia / operation
- Information provision
- Engage in regular review of institutional patient information leaflets
- Risk assessment
- At a minimum, use Nottingham Hip Fracture Score, a frailty score and 4AT score
- Bone Cement Implantation Syndrome
- Read and implement safety guideline (2015) issued by Association of Anaesthetists and British Orthopaedic Association and British Geriatric Society
- See here: https://tinyurl.com/k2yh22j6
- Regional review / oversight
- Participate in peer-review process / informal multi-disciplinary service review programmes
- Participate in peer-review process / informal multi-disciplinary service review programmes
Controversial topics:
Delaying surgery
- 36-hour window: is the suggested maximum time from fracture to surgery
- This is considered sufficient time to proactively correct obstacles to surgery
- Risk of delay contributes to poor outcomes to greater extent than correcting abnormalities to numerical value
- 12-hourly reviews: the advised frequency of anaesthetic assessments if delayed / cancelled
- 7 reasons for delay:
- Haemoglobin < 80g/L-1
- Plasma sodium < 120 or > 150 mmoL-1; Potassium < 2.8 or > 6.0 mmol/L
- Uncontrolled diabetes
- Uncontrolled or acute onset left ventricular failure
- Correctable cardiac arrhythmia with ventricular rate > 120.min-1
- Chest infection with sepsis
- Reversible coagulopathy
Echocardiography
- Do not delay surgery pending echocardiography
- Despite quantifying the nature of valvular heart disease and impairment, any treatment is unlikely to precede surgery
- Favour careful administration of invasively monitored general or spinal anaesthesia
- If suspected / known valvular heart disease, consider short-term, post-operative admission to higher-care unit (i.e., HDU / ICU)
Anticoagulation / antiplatelets
- Includes an associated guideline : https://tinyurl.com/5dnz7u4t
- Use is associated with slightly increased risk of perioperative blood transfusion, but nil increase in mortality
- Balance the risk and benefit of vertebral canal haematoma from neuraxial blockade against risk of general anaesthesia on an individual basis
- These medications flag serious cardiovascular pathology – be mindful that abrupt pre-operative cessation and / or delay to re-commencement post-operatively increases risk of cardiac ischaemia and stent occlusion, cerebrovascular accident, and limb ischaemia
- High risk patients include those on dual antiplatelet therapy, and those who recently commenced therapy (i.e., within 6-months of initiation)
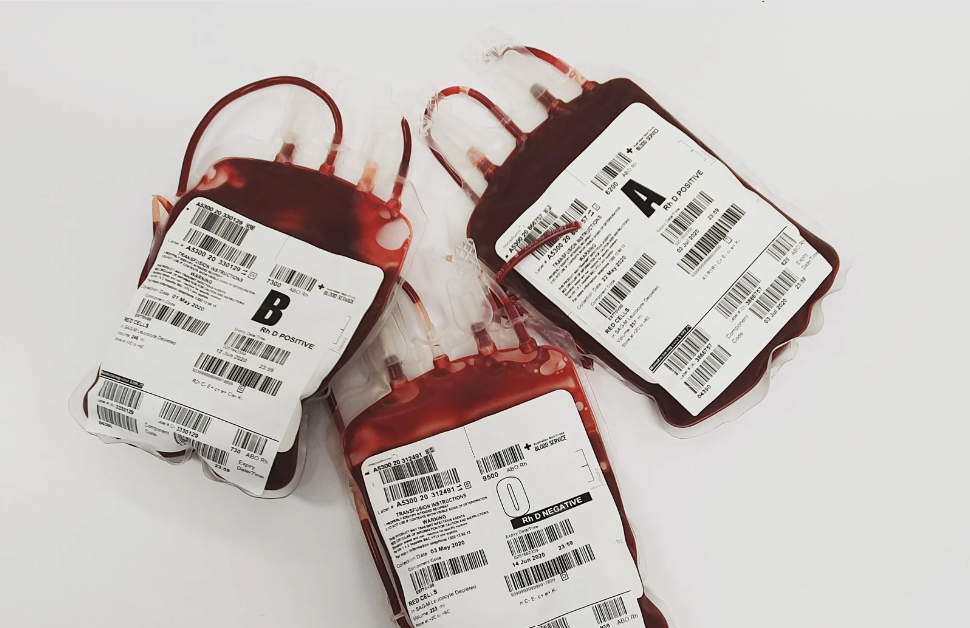
Perioperative blood transfusion
- Aim Hb > 90g/L-1 or > 100g/L-1 in frailer patients (e.g., history of IHD, post-op fatigue/dizziness limiting re-mobilisation)
- Tranexamic acid: use as per hospital policy – may reduce transfusion requirements, however nil strong evidence for improved outcomes, nor risk of thrombosis
Discharge destination
- Access to higher-level care (e.g., HDU / ICU) should not be denied on the basis of age or presence of hip fracture
- Communicate intraoperative care with orthogeriatric colleagues and ward staff
Research, audit and quality improvement:
- Focus is shifting from mortality and length-of-stay to patient-centred functional outcomes and quality-of-life
- The guideline provides (Appendix) a set of 10 research priorities to direct future endeavours
More than hips:
The guideline can also be used to guide management of long-bone and periprosthetic fractures
Appendix S1: Anticoagulation / Antiplatelets:
Suggested management of hip fracture patients taking anticoagulant or antiplatelet medication
Antiplatelets
Single agent use is not a contraindication to spinal anaesthesia
Dual agent use is not an absolute contraindication to spinal anaesthesia (however the risks/benefits should be strongly against general anaesthetic)
Monitor all high-risk patients for signs of vertebral canal haematoma
– e.g., back pain, numbness, motor weakness, bladder / bowel incontinence
Warfarin
Admission and pre-operative period
- If for uncomplicated AF / DVT / PE then stop Warfarin, check INR and give Vitamin K
- Re-check INR 4 to 6-hours later
- INR 1.5, proceed with surgery
- INR > 1.5 consider further Vitamin K or other reversal agent as per hospital policy
Surgery and anaesthesia
- INR 1.8 proceed with surgery
- INR 1.5 proceed with neuraxial anaesthesia
- If no active bleed, recommence Warfarin 12- t0 24-hours postoperatively (consider bridging with low molecular weight heparin)
*Consult haematology if anticoagulated for other reasons (e.g., mechanical mitral valve)
Direct oral anticoagulant drugs (DOACS)
Consider risk (surgical haemorrhage / vertebral canal haematoma / thromboembolism) and benefit (timely surgery)
Wait two half-lives between the last dose and surgery / anaesthesia
Half-life and waiting time
*assuming healthy elderly patient with creatinine clearance : 30 ml.min-1 (Cockcroft-Gault)
- Dabigatran 15-hours x 2 = 30-hour wait
- Apixaban 12-hours x 2 = 24-hour wait
- Edoxaban 12-hours x 2 = 24-hour wait
- Rivaroxaban 12-hours x 2 = 24-hour wait
Restart DOAC 12- to 24-hours postoperatively if nil active bleeding
Table: Anticoagulation / Antiplatelet guiding table from S1 Appendix
|
Drug |
Elimination half-life |
Management |
Acceptable to proceed with spinal |
|
Aspirin |
Irreversible effect on platelets |
Proceed with surgery |
Continue |
|
Clopidogrel |
Irreversible effect on platelets |
Proceed with surgery under GA Monitor blood loss Consider platelet transfusion if concerns regarding bleeding |
Yes, if GA poses greater risk to patient |
|
Ticagrelor |
8–12 h |
Proceed with surgery with GA Monitor for blood loss Consider platelet transfusion if concerned about risk of bleeding |
Yes, if GA poses greater risk to patient |
|
Unfractionated i.v. heparin |
1–2 h |
Stop i.v. heparin 2–4 h pre-op |
4 h |
|
Low molecular weight heparin subcutaneous prophylactic dose |
3–7 h |
Last dose 12 h pre-op |
12 h |
|
Low molecular weight heparin subcutaneous treatment dose |
3–7 h |
Last dose 12–24 h pre-op. Monitor blood loss |
24 h |
|
Warfarin |
4–5 days |
5 mg vitamin K i.v. and repeat INR after 4 h Consider repeating. Consider prothrombin complex for immediate reversal |
If INR < 1.5 |
|
Dabigatran |
15–17 h |
Consider surgery 24–48 h after last dose Review renal function Consider idarucizumab for immediate reversal |
24–36 h if TT or dabigatran assay normal. If TT abnormal (prolonged) or assay > 50ng.ml-1, give idarucizumab and proceed. |
|
Rivaroxaban Apixaban Edoxaban |
12 h |
May be partially reversed with prothrombin complex. Consider surgery 12–24 h after last dose* Review renal function (*Consider at 12 h under general anaesthesia if bleeding risk acceptable) |
24 h if CrCl ≥ 30 – no assay 48 h if CrCl < 30 – Or if available, proceed if DOAC specific assay ≤ 50 ng.ml-1 or reverse if DOAC specific assay > 50 ng.ml-1 |
|
GA, general anaesthesia; i.v., intravenous; TT, thrombin time; CrCl, creatinine clearance (Cockcroft-Gault) |
|||
Other contents of S1 appendix include:
- Post-anaesthesia care unit (PACU) discharge proforma
- Standardised hip anaesthesia routine protocol (SHARP)
- Research recommendations
- Quality assurance / improvement (QA/QI) toolkit
Strength:
This guideline is something of a one-stop-shop for perioperative management of hip fractures. It provides guidance for aims of care with an acknowledgement to developments in evidence and consensus since the 2011 guideline.

Weakness / areas for consideration:
Lack of associated research
More an area of consideration rather than intrinsic weakness, the authors acknowledge a relative lack of RCTs into the specifics of anaesthetic perioperative management of hip fractures.
Standardisation of anaesthetic care
Again, more an area of encouragement featured throughout the guideline, for anaesthetic departments to protocolise/standardise the care of hip fractures based on this, and associated guidelines.
Population / system bias
While fair to assume some equivalence between the UK’s health service and population with other countries, it’s important to consider possible limitations in the guideline’s application in areas of differing resource availability.
Take home:
Management of our 80-year-old patient with fractured NOF on Warfarin is directed by the indication (i.e., as per guideline above +/- haematology consult if for something other than uncomplicated AF, DVT/PE i.e., mechanical mitral valve) INR targets, and associated reversal with Vitamin K / Prothrombin complex. We may proceed with neuraxial anaesthesia if the INR is < 1.5, and there will be appropriate post-operative follow-up for signs of vertebral canal haematoma. Aim to re-commence Warfarin 12- to 24-hours postoperatively if there is no active bleeding and consider use of bridging low-molecular weight heparin.
Overall, this article covers a clinical area of great individual and public health significance by providing evidence-based advice and guidelines around perioperative hip fracture management. Its attention to new foci – and commentary on areas of ongoing contention – gives us confidence and tools to invest in the care of a vulnerable patient population.
Further reading:
S1 Appendix
https://tinyurl.com/5dnz7u4t
Australian & New Zealand Hip Fracture Registry report (ANZHFR) 2022
https://anzhfr.org/registry-reports/
(UK) National Hip Fracture Database Report (NHFD) 2022
https://www.nhfd.co.uk/docs/reports2021