By Dr Wendell Zhang
Key Takeaways
-
Laparoscopic surgeries improve patient outcomes
-
Anaesthetists should be aware of and plan for common physiological changes associated with laparoscopic surgeries, particularly those during position changes and abdominal cavity insufflation
-
A comprehensive preoperative assessment may be necessary for those with reduced physiological reserve from cardiorespiratory comorbidities

Preamble
You are a medical student on the first day of your anaesthetics rotation. In front of you is Ms Taylor, a 47-year-old woman who is about to have a laparoscopic cholecystectomy.
The supervising anaesthetist gives you a pat on the back once you finish securing the endotracheal tube and the case gets underway. Just as you’re collecting yourself after that nerve-wracking job, you hear the anaesthetist ask you:
“What are the physiological implications of undergoing a laparoscopic procedure?”
A brief introduction to laparoscopic surgery:

To answer this loaded question, let’s explore some basic concepts of a laparoscopic procedure.
Laparoscopic surgery, colloquially known as “keyhole surgery”, first involves several small incisions in the abdomen or pelvis. These incisions facilitate the insertion of trocar “ports” through which various instruments may be inserted to perform minimally invasive surgical and diagnostic procedures in the abdominal cavity.
Why laparoscopic surgery?
There are many different procedures which may be performed with laparoscopic technique, with some of the most common including:
-
Appendicectomy
-
Cholecystectomy
-
Fundoplication
-
Bowel resection
-
Hernia repair
The list is constantly expanding due to the attractive benefits of the laparoscopic technique
There a several advantages and disadvantages to using a laparoscopic approach to perform these procedures:
|
Advantages |
Disadvantages |
|
|
Insufflation of the Abdomen
Following the insertion of the trocars, the abdominal cavity is insufflated with gas. This is typically carbon dioxide (CO2) although other gases such as helium, argon, nitrous oxide, and nitrogen may be used.
While there is little conclusive evidence demonstrating the superiority of any gaseous insufflation over the others, (CO2) is the most widely used in Australian centres. CO2 is inexpensive, readily available, inflammable and relatively soluble in blood.
|
Pros of CO2 abdominal insufflation |
Cons of CO2 abdominal insufflation |
|
|
After obtaining access through the abdominal wall, the abdominal cavity is insufflated to around 12-15mmHg with carbon dioxide at a rate of approximately 4-6L/min. This pressure is maintained throughout the operation with a steady stream of gas via the ports.
The abdominal insufflation provides the surgeons the space to visualise and manipulate the intra-abdominal viscera but ultimately creates a supraphysiological intra-abdominal pressure.
Patient Positioning
The positioning of the patient on the bed is also variable depending on the target of the operation. Typically, this is tailored to better visualise the viscera using the effects of gravity to isolate the target region. Depending on the surgeon’s preferences, the positioning of the patient in each of these procedures may vary.

For a laparoscopic appendicectomy, the patient is typically placed supine, in the Trendelenburg (head down) and may be rotated to the left.
For a laparoscopic cholecystectomy, the patient is again placed supine but in the Reverse Trendelenburg (head up) with some rotation to the left.
The focus of the discussion on physiological impacts will be centred upon these two operations as they are the most frequently encountered laparoscopic operations in most surgical centres.
To help contextualise these concepts, we will be taking the ABCDE approach to understanding the physiological effects of laparoscopic surgery.
The altered physiology of abdominal insufflation:
Abdominal insufflation is one of the key defining features of laparoscopic procedures and as such, ought to be discussed first. Most of these physiological changes are present at the expected intra-abdominal pressures during laparoscopic surgery but may become more pronounced if the pressure is inadvertently raised.
|
Physiological implications of abdominal insufflation with CO2 |
|
|
A |
|
|
B |
|
|
C |
|
|
D |
|
|
E |
|
Airway
Aspiration risk
Abdominal insufflation leads to increased intra-abdominal pressure which in turn will lead to increased pressure against hollow viscus. The resting tone of the lower oesophageal sphincter may already be partially compromised from the pharmacological effect of agents used to induce a general anaesthetic (such as opioids). The increased pressure against the stomach may cause regurgitation of stomach contents and lead to an aspiration event
Breathing
Higher peak pressures
Abdominal insufflation and the subsequent rise in intra-abdominal pressure causes cephalad pressure (in the direction of the head) on the diaphragm and may reduce intra-thoracic volumes. This opposing force makes it harder for the lungs to expand and simultaneously reduces the overall compliance of the lungs and increases pulmonary airway resistance.
Consequences of this include the requirement of higher peak airway pressures to achieve adequate minute ventilation. Prolonged high airway pressures can cause damage to the alveoli and cause widespread barotrauma.
Reduced Functional residual Capacity
The constant cephalad pressure also may result in a loss of the functional residual capacity (FRC) of the lungs. The FRC is defined as the volume remaining in the lungs after a normal tidal exhalation. This also represents the point at which the forces of elastic recoil of the lung and the forces of outward expansion of the chest.
The FRC is important as it serves as a reserve of O2 within the lungs. When the lung is at the FRC, the tension in the lung tissue will splint the small airways open. Maintaining an FRC is also important as it reduces pulmonary vascular resistance by preventing the mechanical compression of pulmonary vasculature.
Thus, when the FRC is reduced by an upwards intra-abdominal force, there is a reduced O2 reserve, there is basal atelectasis from the collapse of airways and subsequent shunt, and there is an increase in pulmonary vascular resistance.
Subcutaneous emphysema
Furthermore, there is a risk of developing subcutaneous emphysema during laparoscopic surgery which can serve as a continuous reservoir of CO2.
CO2-mediated acidosis
In addition, the insufflation of the abdomen with CO2 leads to hypercarbia as CO2 is absorbed into tissue before subsequently entering circulation. Carbon dioxide’s high solubility means there is a high potential for CO2 to accumulate in body tissue.
From a respiratory standpoint, this hypercarbia necessitates an increased minute ventilation. In addition, the acidosis caused by the hypercarbia also results in a reduced oxygen-carrying capacity of haemoglobin which can lead to poor oxygenation of vital organ systems.
CO2 embolism
A rare complication of laparoscopic surgery is carbon dioxide embolism where a pocket of gas enters the circulatory system and can often be deposited and obstruct the pulmonary vasculature. Similar to other pulmonary embolic phenomena, this can lead to severe cardiorespiratory compromise.
Cardiovascular
Abdominal insufflation in laparoscopic surgery can have profound impacts on a patient’s cardiovascular physiology. The overall impact depends on the insufflation pressure and the cardiovascular state and function of the patient.
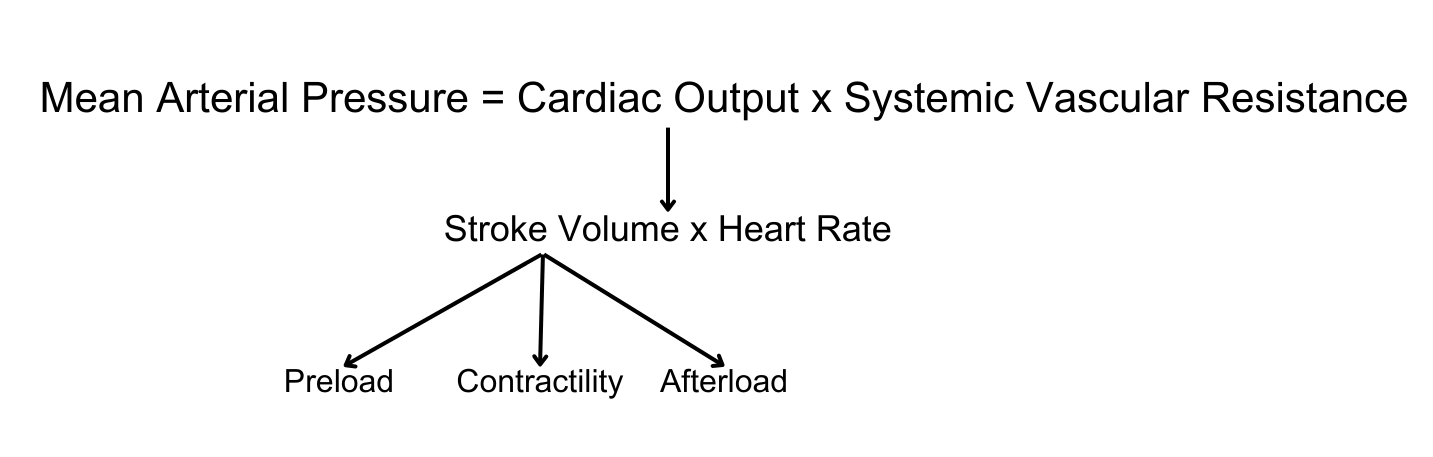
Preload
With the initial stages of abdominal insufflation, there may be a noticeable increase in cardiac output as compression of the abdominal venous systems increases venous return.
With prolonged raised intra-abdominal pressures, the venous return decreases as the major veins collapse and blood pools in the peripheral venous circulation.
Afterload
In addition, increasing intra-abdominal pressures also leads to increased afterload due to compression of intra-abdominal tissues and arteries. In particular, this compression and altered physiological state can prompt the activation of various neuroendocrine systems (including RAAS, vasopressin and sympathetic nervous system) which may act to further increase peripheral vascular resistance while seeking to preserve cardiac output.
Right Ventricular Function
The haemodynamic state induced by pneumoperitoneum may also place increased stress upon the right ventricle. In addition to receiving less preload, the factors increasing pulmonary vascular resistance also increase the afterload on the right ventricle.
Vagal Stretch Reflex
A rare complication of rapid insufflation of the abdomen is the vagal stretch reflex. In conjunction with the use of sympatholytic medications such as opioid analgesia, this can potentially lead to bradyarrhythmias and even asystole.
Disability
CO2-mediated cerebral vasodilation
An increase in arterial CO2 during laparoscopic surgeries causes dilation of cerebral blood flow via the action of the H+ ions on the smooth muscle cells in the vessel walls. This can significantly increase intracranial pressure and cause subsequent neurological complications in patients at risk.
Everything else
Impaired organ perfusion
The impact of the raised intra-abdominal pressure causes increased resistance in renal vasculature, thereby impairing renal circulation. In addition, the activation of the sympathetic nervous system and RAAS system may further cause renal vasoconstriction. In patients with pre-existing renal impairment, this may precipitate an acute kidney injury.
The mechanical effects of raised intra-abdominal pressure and the heart’s reduced cardiac output state can also lead to a reduction in splanchnic circulation during laparoscopic surgeries. In prolonged surgeries, this may lead to acute ischaemic injury to bowel tissue.
Patient Positioning
In addition, the positioning of the patient also impacts their physiological state. The changes here are primarily driven by the effects of gravity.

|
Head Up (Reverse Trendelenburg) |
Head Down (Trendelenburg) |
|
|
A |
|
|
|
B |
|
|
|
C |
|
|
|
D |
|
|
|
E |
|
|
Airway
Aspiration & dependent oedema
The Trendelenburg position (head down) increases the likelihood of aspiration events as gastric contents can migrate due to the effects of gravity. In addition, the repositioning of a patient into this position can lead to an upward migration of the airway device if improperly secured.
Furthermore, prolonged Trendelenburg positioning can compromise the venous drainage of tissue in the head and neck. This can lead to upper airway oedema which may complicate any efforts to re-establish a protected airway.
Breathing
The impacts of patient positioning on respiratory dynamics share many similarities with the mechanisms discussed from the effects of a pneumoperitoneum. For patients in the Trendelenburg position, especially those on a steep incline, the contents of the abdomen will place cephalad pressure on the diaphragm resulting in the aforementioned physiological changes.
Circulation
The impacts of patient positioning on cardiac output are primarily driven by venous return. In the Trendelenburg position, patients have increased venous return owing to the effects of gravity. This increases cardiac output but may simultaneously increase pulmonary arterial pressure. In the reverse Trendelenburg position, the inverse occurs as there is reduced venous return.
Disability
The positioning of the patient, especially over long periods, may impact their cerebral perfusion. Patients in the Trendelenburg position have reduced venous return from their head and neck due to the effects of gravity. Over time, this can cause oedema in cerebral tissue and increase intracranial pressure.
Everything else
Increased intraocular pressure
A further consequence of reduced venous drainage is that patients in the Trendelenburg position may have increased intraocular pressures which can result in worsening glaucoma, retinal pathology and loss of visual acuity post-operatively.
Venous Thromboembolism risk
Prolonged reverse Trendelenburg may also slightly increase the risk of developing an intraoperative venous thrombosis owing to the reduced lower limb venous return in this position.
Who may be at increased risk during a laparoscopic procedure?

Given the physiological challenges imposed not just by a general anaesthetic but also by the specific operating conditions in laparoscopic surgery, patients with certain comorbidity characteristics may be at increased risk of decompensating during this procedure.
|
System |
Patient Characteristics |
Complication |
|
A |
Pregnant patients |
Certain positioning can increase upper airway oedema |
|
B |
Severe COPD |
Rupture of bullae from increased airway pressures |
|
Pulmonary Hypertension |
Further elevation of pulmonary vascular pressures can lead to acute right ventricular decompensation |
|
|
Morbid Obesity |
Further increases in intra-abdominal pressures lead to worsening VQ mismatch and hypoxia |
|
|
C |
Ischaemic Heart Disease |
Increased oxygen demand may result in perioperative ischemic complications |
|
Heart Failure |
Sudden increases/decreases in preload can cause acute decompensation with fluid overload or cardiogenic shock |
|
|
Severe aortic stenosis |
Patients with a fixed flow valve (unable to generate higher cardiac outputs) may be at risk of acute cardiac decompensation |
|
|
D |
Chronic Kidney Disease |
Further reductions to eGFR can precipitate an acute kidney injury |
References
Hayden P, Cowman S. Anaesthesia for laparoscopic surgery. Continuing Education in Anaesthesia, Critical Care & Pain. 2011 Oct 1;11(5):177-80.
Atkinson TM, Giraud GD, Togioka BM, Jones DB, Cigarroa JE. Cardiovascular and ventilatory consequences of laparoscopic surgery. Circulation. 2017 Feb 14;135(7):700-10.
Knight DJ, Mahajan RP. Patient positioning in anaesthesia. Continuing Education in Anaesthesia, Critical Care & Pain. 2004 Oct 1;4(5):160-3.
Lee-Ong A. Physiologic Considerations in Laparoscopic Surgery. InMastering Endo-Laparoscopic and Thoracoscopic Surgery: ELSA Manual 2022 Nov 17 (pp. 83-85). Singapore: Springer Nature Singapore.
Park EY, Kwon JY, Kim KJ. Carbon dioxide embolism during laparoscopic surgery. Yonsei medical journal. 2012 May 1;53(3):459-66.
Fahy BG, Barnas GM, Nagle SE, Flowers JL, Njoku MJ, Agarwal M. Effects of Trendelenburg and reverse Trendelenburg postures on lung and chest wall mechanics. Journal of clinical anesthesia. 1996 May 1;8(3):236-44.
Gao D, Sun L, Wang N, Shi Y, Song J, Liu X, Yang Q, Su Z. Impact of 30° Reserve Trendelenburg Position on Lung Function in Morbidly Obese Patients Undergoing Laparoscopic Sleeve Gastrectomy. Frontiers in Surgery. 2022 Feb 24;9:792697.
Kalmar AF, Foubert L, Hendrickx JF, Mottrie A, Absalom A, Mortier EP, Struys MM. Influence of steep Trendelenburg position and CO2 pneumoperitoneum on cardiovascular, cerebrovascular, and respiratory homeostasis during robotic prostatectomy. British journal of anaesthesia. 2010 Apr 1;104(4):433-9.
Holzheimer RG. Laparoscopic procedures as a risk factor of deep venous thrombosis, superficial ascending thrombophlebitis and pulmonary embolism-case report and review of the literature. European journal of medical research. 2004 Sep 29;9(9):417-22.